AARP Hearing Center


For decades, as Americans approached their 65th birthday, all they had to do to get Medicare, the nation’s government-sponsored health insurance for older adults, was sign up. The program wasn’t all that complicated. You went to the doctor armed with your Medicare card. Your physician or hospital took care of you and billed Medicare. Then you — or the supplemental (Medigap) plan you bought — paid your out-of-pocket share. Easy.
Today’s Medicare isn’t your grandparents’ program. New enrollees have an immediate big decision to make: Should they enroll in original Medicare (also referred to as traditional Medicare) or sign up for the private insurance managed care alternative, Medicare Advantage (MA)? The two options not only differ in how they operate but increasingly in what coverage and services they provide. Making the decision requires looking down two roads that more and more are heading in different directions.
Original Medicare’s biggest draw remains the freedom enrollees have to go to any doctor or hospital in the country that takes Medicare. In most cases, you don’t need a referral to go to a specialist or get a covered procedure done. It’s a simple fee-for-service insurance structure that was once commonplace across America but has mostly vanished for those under 65.
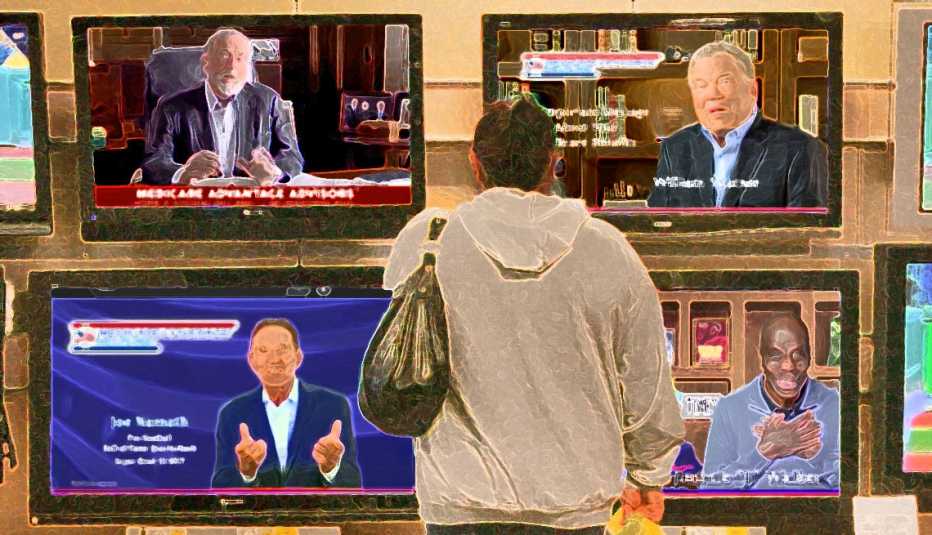
In Medicare Advantage, plans can feel more familiar, as they closely resemble the managed care plans offered by many employers, often in the form of a health maintenance organization (HMO) or preferred provider organization (PPO). An MA plan is the one-stop-shopping alternative that bundles hospital, doctor and prescription drug coverage. Most offer extra benefits not in original Medicare. MA plans also cap how much beneficiaries must pay out of pocket each year, something original Medicare does not.
Another big difference: Original Medicare is managed entirely by the federal government (oversight by Congress, day-to-day operations by the Centers for Medicare & Medicaid Services (CMS), meaning it is not operated for a profit. Advantage plans, by contrast, are operated by private and often for-profit organizations that get flat-rate payments from the government to provide health care to an enrollee. By managing costs and a patient’s care carefully, they can — in theory — provide all needed services and still have money left over for their bottom line.
MA’s promise of extra benefits and lower premiums has been effective. In 2008, only 22 percent of beneficiaries were in Advantage plans. Since then, enrollment in these managed care plans has more than doubled and continues to grow. In 2023, more than half of Medicare’s 60 million beneficiaries who have both Medicare parts A and B are enrolled in an MA plan.
The future path
Medicare now finds itself at a crossroads. Based on current patterns, it won’t be long before enrollment in MA plans substantially overtakes enrollment in original Medicare. Does the original need to be changed to remain competitive with MA? More fundamentally, will original Medicare as envisioned by President Lyndon Johnson and Congress in 1965 cease to exist in the years to come?
“I genuinely do believe that the future of Medicare lies in Medicare Advantage,” says James E. Mathews, executive director of the Medicare Payment Advisory Commission (MedPAC), established by Congress to analyze the program and provide advice. Mathews expects there will be a “natural migration” to MA, but he’s not sure whether that means original Medicare will disappear. “It remains to be seen whether there is going to be some subset of the Medicare population for whom Medicare Advantage simply will not work.”
AARP spoke with advocates and current and former Medicare leaders who uniformly say it’s not time to pull the plug on original Medicare, now or in the near future.
Preserving and strengthening Medicare is one of AARP’s key policy concerns. That includes maintaining original Medicare. “We strongly believe that traditional Medicare should be protected and strengthened and that there has to be a level playing field between traditional Medicare and Medicare Advantage,” says Megan O’Reilly, AARP vice president for health and family issues.
CMS Administrator Chiquita Brooks-LaSure oversees all Medicare operations. She says her priority is to strengthen both options. “I believe it’s critical that people have a choice between traditional original Medicare and Medicare Advantage,” Brooks-LaSure said in an interview with AARP.
Even experts who are most bullish on Medicare Advantage say they don’t expect original Medicare to go away. The main reason is choice.


The case for keeping original Medicare
Under original Medicare, you can go to any doctor, lab or hospital in the U.S. that participates in the program (about 90 percent of medical professionals do). In MA plans, enrollees mostly must go to providers within the plan’s network, and these networks are highly regionalized. Going out of network means facing a much higher copay for each visit. In some cases, the care may not be covered at all.
“There are always going to be a lot of people who are going to say, ‘Look, I want to go to a doctor I want, and I don’t want to be limited,’ ” says Tom Scully, who was CMS administrator from 2001 to 2003 and is a supporter of Medicare Advantage. As a result, “I think original Medicare will never go away.”
For Arizonan Patrick Witter, a wider choice of medical providers was why he chose original Medicare. The 73-year-old retired educator says the freedom of choice and the ability to have a long-term relationship with his doctors are what’s most important. “I’ve been seeing my urologist for 14 years,” says Witter, a survivor of bladder cancer. “I’ve been seeing the same cardiologist since 1995 when they saved my life and put a stent in my heart. There’s a certain amount of loyalty and trust with those doctors who you know both professionally and, in many ways, personally.”
Until they enroll, many Americans don’t realize how costly and complicated Medicare can be. That is especially true if you choose original Medicare. Most original enrollees must make three regular insurance payments: one for basic Part B coverage, one for a Part D prescription plan, and one more for a Medigap policy to cover some or all of the expenses that Medicare doesn’t. And there are other expenses on top of the premiums; for example, original Medicare Part B has an annual deductible ($226 in 2023); there’s also a deductible for every hospital visit, which in 2023 is $1,600. Those charges take a heavy financial toll.
By contrast, an Advantage plan enrollee usually has just one recurring payment: It includes the government-mandated Part B coverage cost and, in some cases, a small additional premium, which varies by what plan you choose and where you live. You pay various copays and deductibles for your services and doctor visits, but the rest is fully covered by the plan, and you know going in what the copay is for the different providers. Costs under MA can also add up, though, especially if you need hospital care; most plans have a per-day hospital charge.









































































More on Medicare
Medicare Part D Premium Changes for 2024
The average monthly prescription drug charge to fall nearly $1
How Medicare works after a public service career
Retired government workers and military members have choices to makeBy Dena Bunis