AARP Hearing Center

The Food and Drug Administration (FDA) has green-lit two blood tests that can help doctors diagnose Alzheimer’s disease, which, as the most common form of dementia, affects more than 7 million older Americans and is marked by a decline in memory and thinking skills.
The tests are not screening tools, and they are not intended to provide a definitive diagnosis. However, doctors and Alzheimer’s experts say these breakthrough tests can help improve the diagnosis process and help prevent additional, unnecessary testing in people who are unlikely to have the disease.
The most recently cleared test — known as the Elecsys pTau181 test, approved in October 2025 — measures certain proteins in blood plasma associated with the disease. Its manufacturer, Roche, says it is specifically designed for the primary care setting to help doctors rule out patients who may exhibit symptoms of cognitive decline but are unlikely to have Alzheimer’s.
In May of 2025, the FDA cleared another test, called Lumipulse, which can detect abnormal clumps of protein in the brain, known as amyloid plaques. These plaques disrupt brain cell function and are a hallmark of Alzheimer’s.
PET scans and spinal fluid tests can also detect amyloid plaques and have been used for years to help doctors diagnose Alzheimer’s. But the tests are expensive and, in the case of a lumbar puncture (a.k.a. spinal tap), invasive. They can also be inaccessible for people in rural areas. Blood tests, on the other hand, require only a blood draw in patients 55 and older who are showing signs and symptoms of the disease.
“Having a blood test just makes it so much easier in being able to make a diagnosis of Alzheimer’s disease,” says Dr. Charles Bernick, a neurologist with the Cleveland Clinic Lou Ruvo Center for Brain Health, based in Las Vegas.
AARP Brain Health Resource Center
Find in-depth journalism and explainers on diseases of the brain — dementia, stroke, Parkinson’s disease, mental-health topics. Learn about healthy habits that support memory and mental skills.
People without symptoms shouldn’t test
The newly approved blood tests are only meant for older adults who are experiencing symptoms of Alzheimer’s. What’s more, the FDA says that the results from blood testing should be used in conjunction with “other clinical evaluations or additional tests” to determine treatment options.
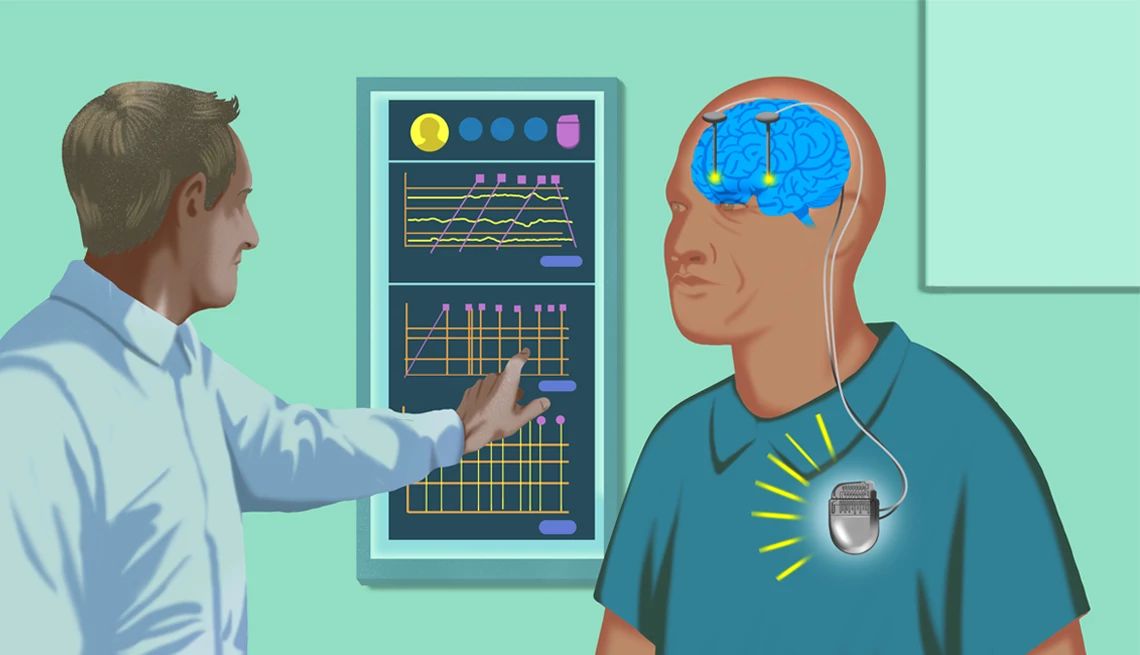
In addition to brain imaging and lumbar punctures, doctors often use neurological exams and cognitive tests, for example, to diagnose a patient with Alzheimer’s. “It still becomes a diagnosis where you have to really look at the whole picture,” Bernick says.
In recent years, the FDA has approved two medications for the treatment of Alzheimer’s — Kisunla (donanemab) and Leqembi (lecanemab). These drugs, which are given by infusion, don’t cure the disease but can help to slow the rate of decline in people in its early stages. Because they work by clearing amyloid plaques from the brain, the presence of amyloid must be confirmed before they can be prescribed.
“They carry some risk. So if you’re going to use them or utilize them, you’ve got to be pretty sure the person has that protein in the brain,” Bernick says. Risks can include swelling and bleeding in the brain.
A blood test for symptoms?
Scientists are hoping that blood tests will one day do more than help diagnose Alzheimer’s disease, but also predict when a person might start experiencing symptoms. Using blood samples from more than 600 adults, researchers analyzed a protein linked to Alzheimer’s disease and built a statistical model to predict symptom onset. The model was able to estimate how many years away a person was from developing thinking and memory problems, with an accuracy of within three to four years. The study’s findings were published in the journal Nature Medicine. For now, the researchers say, such a tool may be useful in clinical trials, since the Alzheimer’s treatments available work best when started in the earlier stages of the disease.






































































)
)






More From AARP
Diagnosing Alzheimer's Before Symptoms?
Early Alzheimer's diagnosis raises treatment concernsLifestyle Changes to Ease Dementia Symptoms
These approaches can support healthy brain aging and prolong everyday functionIs This Normal Memory Loss or Memory Problems?
Tips from experts on how to tell the difference