2024 Deductibles
Part A: $1,632 for each hospital stay in 2024.
Part B: $240 for 2024.
(Some Medigap policies cover Part A and Part B deductibles.)
Part C (Medicare Advantage): Amount varies by plan.
Part D prescription drug plan: Amount varies by plan but cannot exceed $545 for 2024.
Copays
Part C (Medicare Advantage): Amount varies by plan and by service.
Part D prescription drug plan: Amount varies by plan and by prescription.
Coinsurance
Part A: No fee for hospital stays of 60 days or less. For 61 to 90 days, $408 per day for 2024. For 91 days or more, $816 per day or full cost of stay. Medicare also provides 60 “lifetime reserve days” that beneficiaries can use if they need to stay in a hospital for more than 90 days. These can be used only once.
Part B: Typically, 20 percent of the Medicare-approved cost of the service for most services.
Medigap policies typically cover Part A and Part B coinsurance.
Part C (Medicare Advantage): Amount varies by plan and by service.
See more Insurance offers >
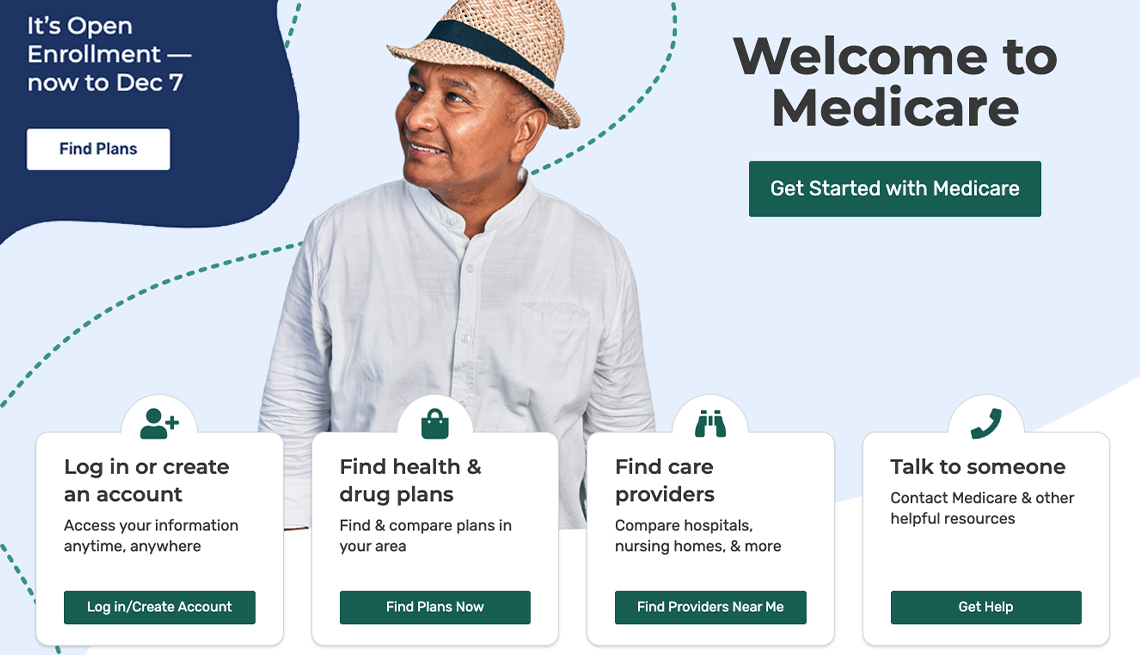
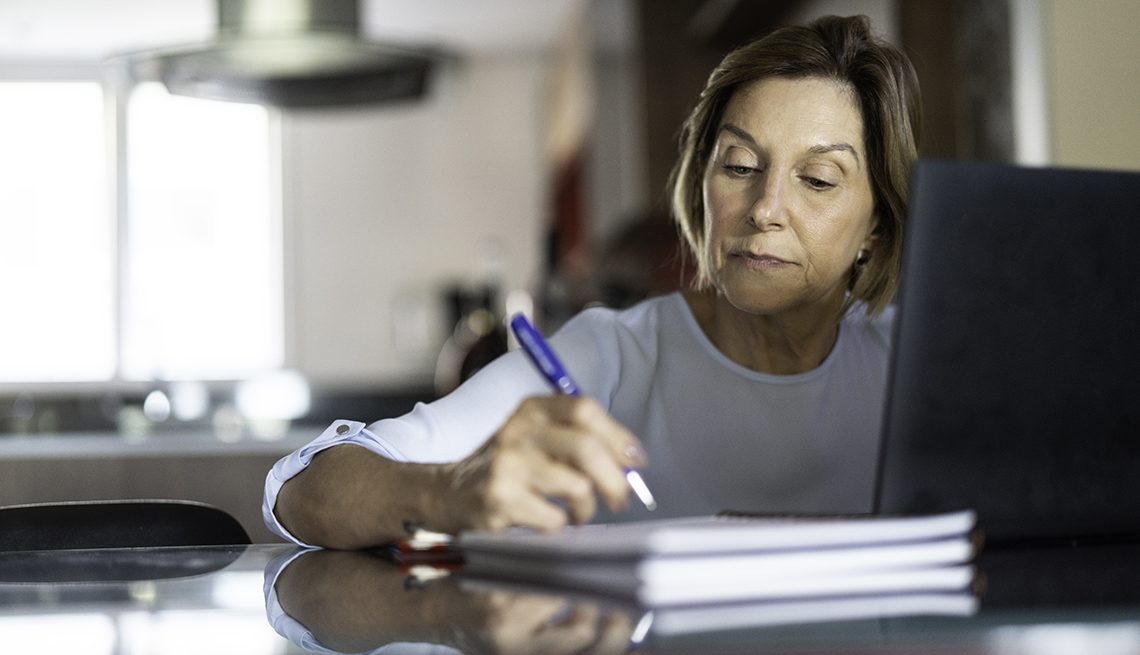
Need help affording Medicare?
Medicare’s out-of-pocket costs — premiums, deductibles, copays and coinsurance — can easily result in a large tab each year. If you’re struggling to meet those expenses, you might be eligible for federal and state assistance.
If you qualify for Medicaid , the federal-state health insurance program for people with low incomes and individuals with disabilities, it will pay some or all of your out-of-pocket expenses. Individuals on both Medicare and Medicaid are known as “dual eligibles.”.
Coronavirus costs
Medicare will still pay for beneficiaries to get vaccinated — including getting boosters — for COVID-19 with no out-of-pocket expenses. The program will also pay for beneficiaries to get tested, with no charges to the beneficiary, although over-the-counter tests are no longer free. You can go to covid.gov/tests and get four free tests mailed to your home.. Medicare will also pay for U.S. Food and Drug Administration-approved COVID-19 treatments, such as Paxlovid.
Other programs are designed for beneficiaries with incomes that are too high to qualify for Medicaid, but who still have trouble paying their health care bills. Each program has specific income and asset limits and eligibility requirements that are adjusted annually.
- The Qualified Medicare Beneficiary (QMB) program helps pay for Part A and Part B premiums as well as deductibles, coinsurance and copays. If you qualify for this program, you automatically qualify for the Extra Help prescription drug program to help you with the out-of-pocket costs of your medicines. This program has the lowest income threshold of the four.
- The Specified Low-Income Medicare Beneficiary (SLMB) program helps pay for only Part B premiums, not the Part A premium or other cost sharing. If your income is too high to qualify for the QMB program, you might qualify for this one. You also automatically qualify for Extra Help for prescription drugs. The Extra Help program is designed to help people with limited resources pay for Part D prescription drug plan premiums, deductibles and copays. You can apply through the Social Security Administration.
- The Qualifying Individual (QI) program helps pay for only Part B premiums, not the Part A premium or other cost sharing. If your income is too high for QMB and SLMB, you might qualify for QI. To get help from this program, you must reapply for benefits every year. Funding is limited, so these benefits are first come, first served. Priority is given to individuals who received help through this program the previous year.
- The Qualified Disabled and Working Individuals (QDWI) rogram helps pay only for Part A premiums. This program is designed for individuals with disabilities who are younger than 65 and currently working.
Your state Medicaid program or State Health Insurance Program — also known as SHIP (877-839-2675 toll-free) — can provide enrollment assistance and more details on the income caps and other eligibility criteria.
Editor’s note: This story has been updated with 2024 information.






















































































More on Medicare
How Much Do You Know About Medicare?
Take this quiz and discover how knowledgeable you are about the health insurance program
Medicare Makes It Easier to Compare Doctors, Health Facilities Online
New interactive tool searches hospitals, nursing homes, rehab, hospice and moreAARP Answers: Medicare and the Coronavirus
The latest on free testing, telehealth, elective surgeries and more