Staying Fit
When you choose original Medicare, health care providers and hospitals send their bills for your care directly to Medicare. The Medicare summary notice (MSN) is a statement that shows all the services and supplies that were billed to the program in the past three months, how much Medicare paid and the maximum amount you may owe a provider.
Similar to an explanation of benefits (EOB) notice you may have received from your pre-Medicare health insurance company, this statement is for your reference and is not a bill. If you haven’t receive any services or medical supplies, you won’t get an MSN for that particular quarter.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
Medicare sends this notice every quarter in which you use Medicare Part A or Part B services. If you sign up for an online Medicare account, you can access the statement on the web and can opt out of the mail version and receive electronic Medicare summary notices (eMSNs). If you don’t want to wait for the quarterly statements, you can review your Medicare claims information each month.
Even though your MSN is not a bill, you should still review it carefully. This claims notice can help you keep track of the care you have received and allows you to monitor your out-of-pocket costs. It also can help you spot errors — and even instances of fraud — on your Medicare account.
How do I read the Medicare summary notice?
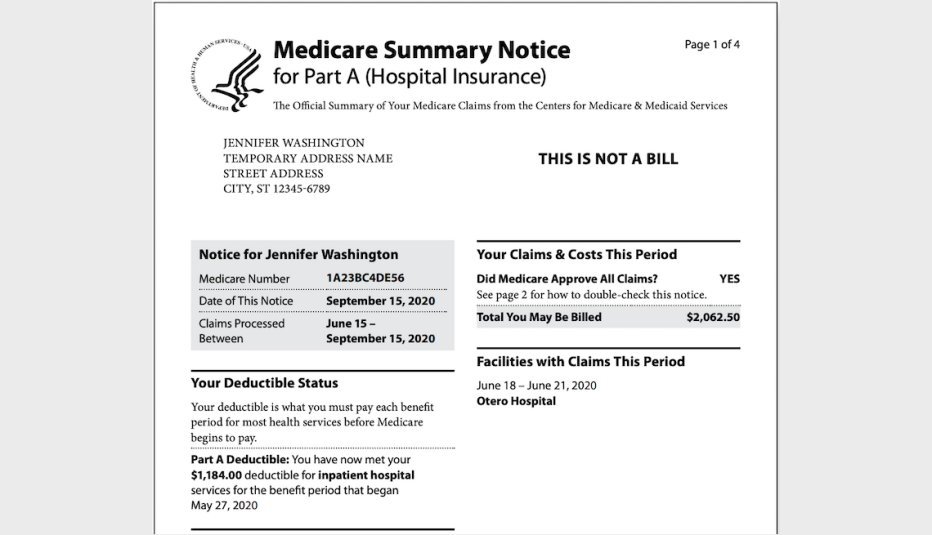
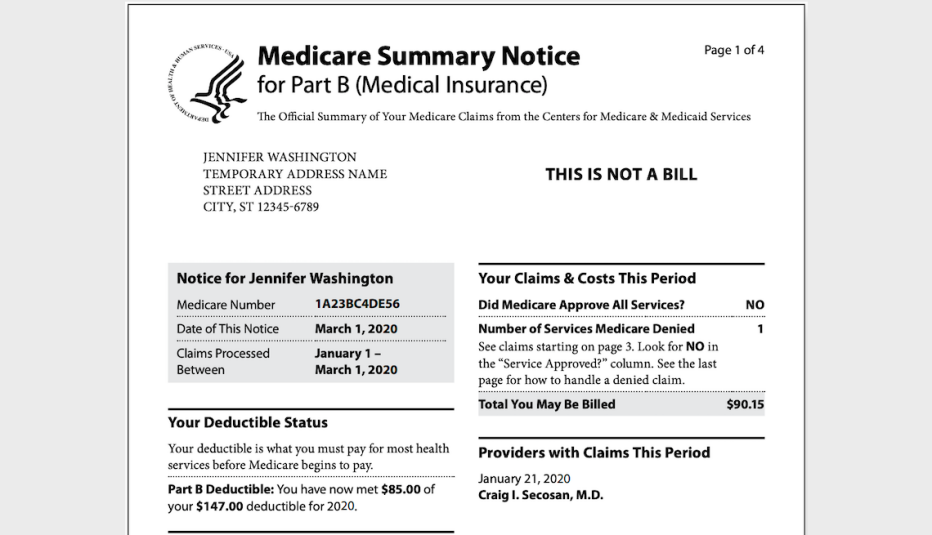
It’s really two notices. You’ll receive a separate MSN for your claims for Part A — which helps pay for inpatient hospital care, inpatient care in a skilled nursing facility, certain home health care services and end-of-life hospice care — and your claims for Part B (which helps cover diagnostic tests, doctors’ services, ambulance transportation and other outpatient costs).
The Part A Medicare summary notice shows the dates of the claims, how much of the deductible you have met, whether Medicare approved all of the claims, and the total amount you may be billed from the facility. It also lists the facilities where you have had claims this period and the dates you received services there.

Page 2 includes tips for reviewing the notice and how many days of coverage you have used in your benefit period for inpatient hospitalization and skilled nursing facilities.
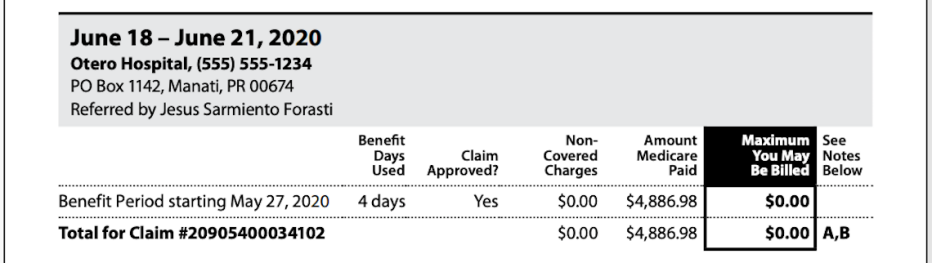
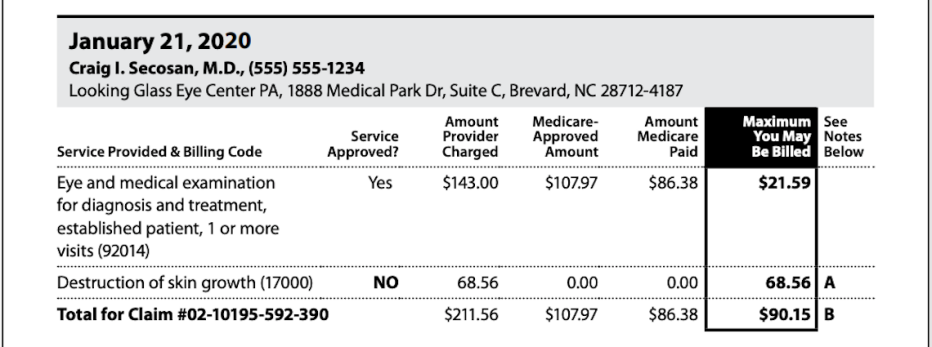
Page 3 provides detailed information about your claim, including the number of benefit days used, whether the claim was approved, any charges that weren’t covered, the amount Medicare paid and the maximum you may be billed. Keep in mind that the bill may be covered by Medigap or other supplemental coverage.
It shows the numbers for the three-month period covered in the summary notice and the total for the claim. It also shows the dates you went to the hospital or facility and when your current benefit period began.

Page 4 explains how to file an appeal if you disagree with a coverage decision, payment decision or payment amount on this notice. It also includes resources for help with filing an appeal, how to file an appeal in writing using the form on the MSN, and the deadline for filing an appeal.

































































More on health
10 Things Medicare Doesn’t Cover
You’ll need to plan ahead to pay for some common medical expenses
Understanding Medicare’s Options: Parts A, B, C and D
Making sense of the alphabet soup of health care choicesHow Much Does Medicare Cost?
Monthly premiums, other out-of-pocket expenses can add up