AARP Hearing Center


More than three times as many Medicare beneficiaries have had access to their regular medical professional over the phone or via a video visit during the COVID-19 pandemic than before the health crisis, according to a new study by the Kaiser Family Foundation (KFF).
In recent years, telehealth visits have become an increasingly popular way for people, especially in rural areas, to have appointments with their medical professionals, but Medicare had limited telehealth coverage benefits. In early 2020, Medicare expanded its coverage of such visits to enable all enrollees to keep up with their medical care while minimizing their exposure risk to the coronavirus. These expanded benefits will continue as long as the COVID-19 public health emergency remains in effect. The emergency was extended in April and no expiration date has been set.
According to the brief from the nonpartisan KFF, the expansion of telehealth benefits has been particularly important to people with disabilities who are low income and among communities of color. This suggests, the study says, “that the temporary expansion of telehealth coverage may be helping some of Medicare's more disadvantaged populations continue to access needed care."
A number of bills have been introduced in Congress that would make permanent some or all of the telehealth expansion for Medicare beneficiaries.
Nearly two-thirds of Medicare beneficiaries report access to Telehealth appointments

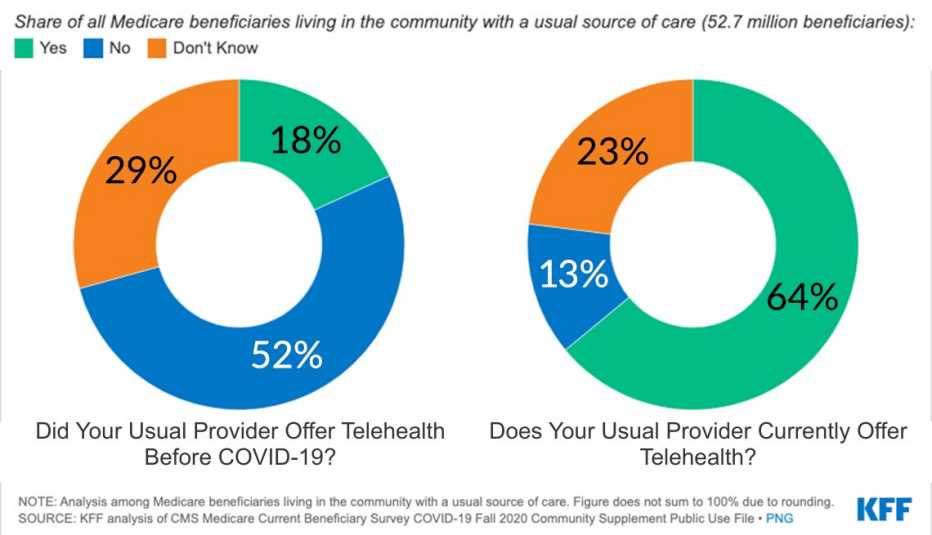
The KFF report was based on the Centers for Medicare and Medicaid Services survey of beneficiaries during the summer and fall of 2020. Some key findings:



































































More on health
How to Get Started With Telemedicine
Ready to make an appointment? We take you through setting one up with your primary care physician or finding a telehealth service
How to Connect With Your Doctor Virtually
Tips for using a smartphone, tablet or computer for telehealth appointmentsAARP Answers: Telehealth and the Coronavirus
How to connect with a doctor and get care from home