AARP Hearing Center

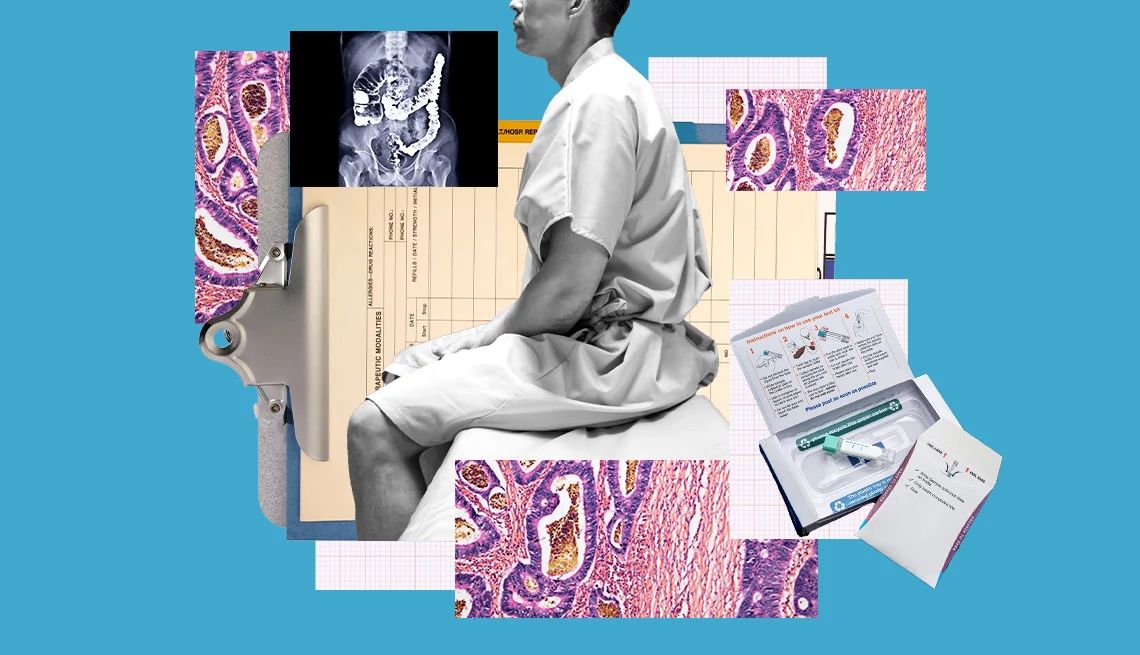
Experts recommend that people at average risk for colorectal cancer start getting screened when they turn 45, but research shows that many adults don’t heed this advice.
According to the Centers for Disease Control and Prevention, about 30 percent of people between the ages of 50 and 75 are not up to date with their colorectal cancer screenings; among adults ages 45 to 49, that share is far greater, according to a study published in the Journal of the National Cancer Institute.
A top reason people skip their screening: Many don’t know that there are tests beyond the colonoscopy, a 2016 American Cancer Society (ACS) survey found. And while it’s considered the gold-standard test, colonoscopy is just one of several tools doctors and patients use to check for colorectal cancer — which, when caught early, is preventable and even curable, says Lance Uradomo, M.D., an interventional gastroenterologist at City of Hope in Orange County, California.
Here’s what you need to know about the different screening options for colorectal cancer, so that you and your doctor can make the best decision for your next screening. Note that if you are at increased risk for colorectal cancer, you may need to start screening before age 45, and you may need specific tests in more frequent intervals.
1. Colonoscopy
Colonoscopy is what doctors consider the gold standard to test for colon cancer and polyps, or growths on the inside lining of your colon or rectum that can turn into cancer.
Warning signs of colorectal cancer
Colon cancer is often asymptomatic for many, but it can have some warning signs. These include a change in bowel habits, bowel pain and blood in the stool.
If you suddenly have trouble going to the bathroom or experience new constipation, that can be a red flag. Constipation is common and can be caused by several factors, such as changes in diet and medications, but if it persists, that can be a cause for concern, says Uradomo.
During the procedure, a gastroenterologist uses a thin, flexible tube with a camera to see inside your colon. If polyps are present, the doctor can remove them and send them for a biopsy. If your test is negative for cancer, you don’t need another colonoscopy for 10 years, according to current screening guidelines.
Like any medical procedure, a colonoscopy is not without risks, including bleeding and reactions to anesthesia. It also requires some prep work to prepare the bowel for the procedure.
Gastroenterologists recommend eating a low-fiber diet two to three days before the colonoscopy. The day before the procedure, you should avoid solid foods and anything red, purple or blue, since these colors can look like blood in the colon. Drinking clear liquids like broth and tea can help you stay hydrated, but you may feel hungry.
Your doctor will order you a prep kit to clean your bowels before the procedure.
2. Blood test
In 2024, the U.S. Food & Drug Administration (FDA) approved a blood test called Shield that, in a large study, detected 83 percent of colorectal cancer found during colonoscopy screenings.




































































More From AARP
Gen Xers Face Higher Cancer Risks
New research highlights troubling trends for younger generationsWhat Your Poop Can Tell You About Your Health
The #1 reason to pay attention to your #2
7 Cancers Linked to Alcohol Use
Accumulating research finds that drinking can raise your risk for several types of cancer