AARP Hearing Center

Researchers at the Mayo Clinic using artificial intelligence (AI) to analyze specific brain activity can detect at least nine different types of dementia. Their aim is faster and more accurate diagnoses, along with the possibility of detecting dementias that are reversible, they say.
“A proper diagnosis can change everything,” says David Jones, M.D., a neurologist who directs the Mayo Clinic’s Neurology Artificial Intelligence Program. “There are many people with dementia-like symptoms that are reversible. This tool enhances the ability to diagnose … these disorders, which is hard for humans to do alone.” That, in turn, makes it more likely patients will get the correct treatments.
The researchers used a tool called StateViewer to correctly identify nine different kinds of dementia (they later ID’d five more), according to a paper published in the journal Neurology. The findings pointed to variations within Alzheimer’s disease, the most common dementia, affecting more than 7 million Americans, as well as Lewy body disease and frontotemporal dementia, according to Jones.
“StateViewer focuses on brain function closely tied to symptoms, so dementias with different symptoms will appear as different forms to StateViewer,” says Jones. This variability is the biological reason why some people with nontraditional forms of Alzheimer’s experience vision problems and go to the eye doctor first; others have speech or language difficulties, and some have issues with executive function, or decision-making, instead of memory loss, he says.
AARP Brain Health Resource Center
Find in-depth journalism and explainers on diseases of the brain — dementia, stroke, Parkinson’s disease, mental-health topics. Learn about healthy habits that support memory and mental skills.
A faster diagnosis with a boost in accuracy
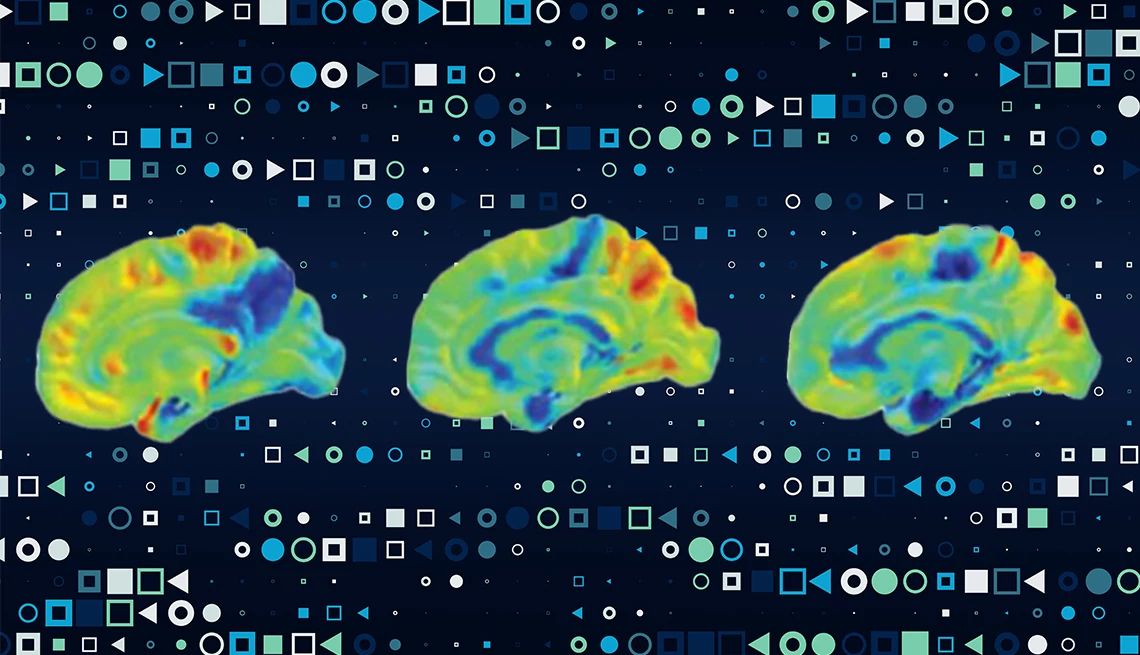
The Mayo scientists trained and tested the AI tool on more than 3,600 scans called FDG-PET (fluorodeoxyglucose positron emission tomography). These scans display brain metabolism, specifically how the brain uses glucose — or sugar — for energy. The tool then compared these scans to a large database of scans from patients with various types of confirmed dementia.
The process of glucose metabolism differs depending on the brain location and the type of dementia, Jones says.
“The patterns are distinctly different from one another,” he says. “[The tool] is looking at which areas of the brain are taking up sugar. These patterns are more subtle than we think. This lack of precision is what makes it hard to treat and why we need AI. To the human eye, they may look similar, but when AI analyzes them, they are clearly very distinct.”







































































More From AARP
Quiz: Vascular Dementia
Test your knowledge of symptoms and treatments
Parkinson's Dementia: Signs and Stages
A decline in thinking and reasoning skills can occur as Parkinson’s progresses
AARP Smart Guide to Keeping Your Memory Sharp
22 science-backed ways to growing a healthier, happier brain, now and in the future