Staying Fit
Money
Get the latest financial news and expert advice on money management to budget effectively, spend wisely, build a nest egg and live well in retirement
Explore Money Topics
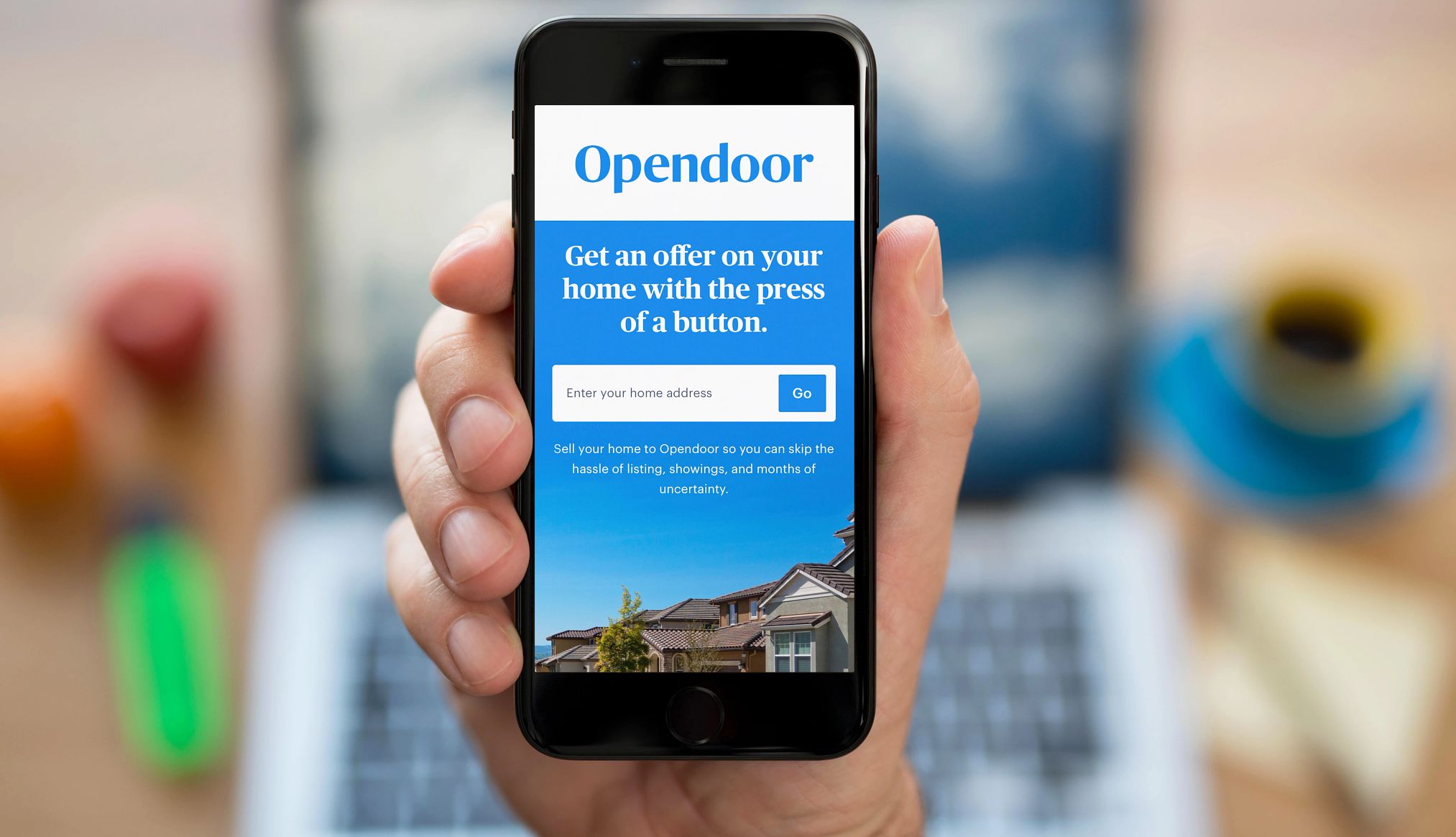
AARP Tools to Manage Your Personal Finances


AARP Membership
$12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
Trending in Money
Recommended for You
AARP IN YOUR STATE
Find AARP offices in your State and News, Events and Programs affecting retirement, health care and more.