Staying Fit
Your doctors and other health care providers must give you an advance beneficiary notice of noncoverage (ABN) if they believe that Medicare won’t pay for items, procedures or other services related to your medical care. This notice, given to you before you receive the care, lists what might not be covered, the reason why Medicare may not pay — and the estimated cost.
Because it comes from your provider, this notice, actually a form, isn’t an official denial from Medicare. But it’s a warning that if you decide to go ahead with a procedure, you’ll probably have to pay the full cost yourself. You must check one of three boxes on the form choosing if you:
- Want the service and want the claim submitted to Medicare.
- Want the service but don’t want the claim sent to Medicare.
- Don’t want the service.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
This notice applies to recipients of original Medicare, which includes Medicare Part A and Part B, but not for private Medicare Advantage plans.
What should I do if I receive an advance beneficiary notice?
You’ll likely get one of these forms in person while you’re visiting your health care provider. But Medicare allows doctors, hospitals or medical equipment suppliers to deliver a copy of the form to a secure fax machine, send the form in the mail, talk to you on the telephone or use email to send you the form. They must give you the form far enough in advance so you have time to consider your options, although the government has not set a specified time period.
They must be able to verify that contact was made directly with you because federal health privacy laws restrict the sharing of certain health information and records.
Don’t ignore the form when you receive it. You’ll need to choose one of the options and sign the form. If you refuse to sign, you might not receive the services you’re expecting.

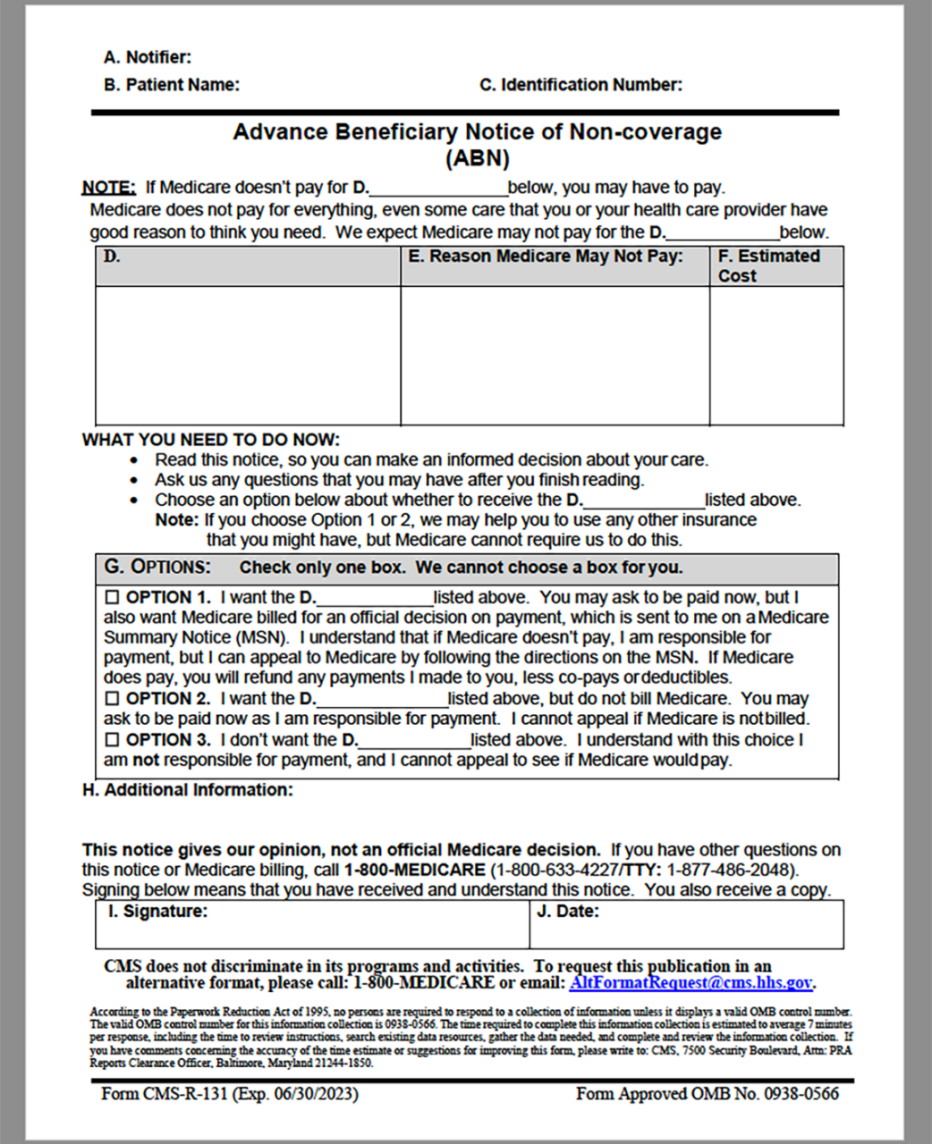
With Option 1, the health care provider will submit a claim to Medicare, but you may have to make some payment in advance. If the federal agency denies the claim as expected, you’ll be responsible for the bill, but you do have a right to appeal a rejection to Medicare.
With Option 2, you stop any attempt for the provider to recoup money from Medicare. You acknowledge that you’ll have to pay for the services and can’t appeal.
With Option 3, you decide you don’t want the services, so you won’t receive them.
The first box on the form is the only one that gives you the right to appeal a denied claim. It also holds out the possibility that Medicare could cover what you want. You may also need to choose the first option if you need proof of a Medicare denial to trigger a payout from secondary insurance that has different coverage from Medicare, such as from an employer or retiree health insurance.
If your secondary insurance is a Medigap policy, it generally won’t pay for services that Medicare denies.
If the claim is submitted to Medicare, you’ll receive a Medicare summary notice, which is similar to an explanation of benefits for other health coverage, letting you know if the claim was approved or denied. This form includes instructions for appealing a claim denial.

































































More From AARP
How do I create a personal online Medicare account?
You can do a lot when you decide to look electronicallyUnderstanding Medicare’s Options: Parts A, B, C and D
Making sense of the alphabet soup of health care choices10 Common Medicare Mistakes to Avoid
Errors can prove costly to new enrollees