Staying Fit

The majority of people who get COVID-19, the illness caused by the new coronavirus, experience mild symptoms, if any at all, and are able to recover at home. But a fraction of the infected population faces a far worse reality — one that can involve severe sickness, even death.
"And right now, we have no good explanation for why,” says Robert Dickson, M.D., an assistant professor in the Division of Pulmonary and Critical Care Medicine in the Department of Medicine at the University of Michigan. “We can't predict which of these patients will basically get the sniffles, and which ones are going to need life support with a mechanical ventilator.”


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
Older adults and people with underlying health conditions are at increased risk for more critical cases of coronavirus, health experts say. Even still, a report from the Centers for Disease Control and Prevention (CDC) shows plenty of young adults also are being hospitalized with difficulty breathing and other life-threatening symptoms.
Coronavirus symptoms
Mild COVID-19 cases:
- Fever
- Cough
- Shortness of breath
People may also experience:
- Chills
- Repeated shaking with chills
- Muscle pain
- Headache
- Sore throat
- New loss of taste or smell
COVID-19 emergency warning signs:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
Source: Centers for Disease Control and Prevention
Here's what happens to the body when a mild case of COVID-19 turns serious:
Inflammation in the lungs makes it hard to breathe
Health experts suspect the coronavirus enters the body through the nose or mouth by way of small droplets that are passed when an infected person coughs or sneezes. Like most respiratory viruses, the infection “seems to start in the upper respiratory tract” — the back of the throat and the nose — and triggers symptoms that are typical of other upper respiratory infections, including fever and cough, Dickson says.
In some people, however, the disease moves down the respiratory tract and settles in the lungs, where it can cause “intense inflammation” (pneumonia) in the tiny air sacs. These sacs are where gas exchange takes place between the lungs and the bloodstream.
Most of the time, this gas exchange — oxygen into the body and carbon dioxide out — occurs easily, Dickson explains. However, “when you have an intense pneumonia, like COVID-19 is causing, those air spaces fill up with pus, they fill up with inflammation,” he says. And thicker pus-filled sacs make it more difficult for oxygen to pass from the lungs into the blood. Essentially: It becomes hard for a person to breathe.
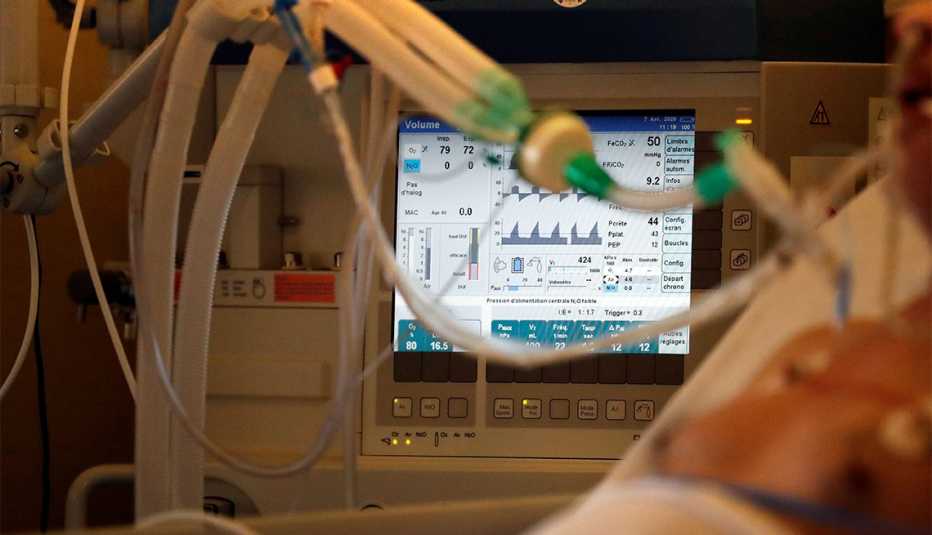
Some patients need help breathing
When a patient starts to experience difficulty breathing, health care providers turn to “a ladder of interventions,” Dickson explains. Sometimes, a few liters of oxygen delivered through a tube that rests below the nose is all a patient needs to recover. If the damage to the lungs is more severe, a higher, faster flow of oxygen can help. In other instances, patients need breathing assistance from a mechanical ventilator.

































































More on health
What Will Getting Coronavirus Treatment Cost You?
Testing may be free, but medical care will likely carry costsHow Veterans Can Get Tested for COVID-19 With VA or Tricare
Non-urgent appointments being rescheduled to handle potential influx of coronavirus casesThe Affordable Care Act Is Helping Fight Coronavirus — But It’s Not Enough
10 years after its passage, many more older adults have health coverage