Staying Fit


In a pandemic filled with grim statistics, one of the grimmest has gone largely unnoticed: 95 percent of COVID-19 deaths in the U.S. have occurred among people who were 50 or older. This even though the majority of coronavirus cases have been reported in people under age 50.
The unnerving numbers don't end there. About 8 in 10 deaths have been among people 65 and older, according to the latest demographic data available from the Centers for Disease Control and Prevention (CDC). Overall, in just a matter of months, the coronavirus has infected 9 million Americans and killed more than 229,000.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
"It's devastating, what's happening,” says Sharon Inouye, a professor of medicine at Harvard Medical School and a geriatrician at Hebrew Senior Life in Boston.

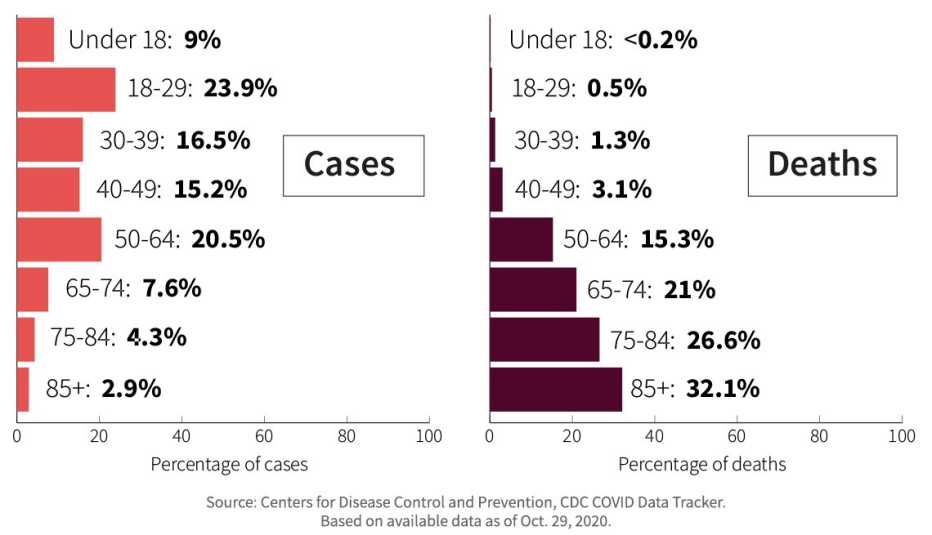
The 95 Percent
Coronavirus cases and deaths by age group
Warning signs emerged early
It was an already trying spring evening — at the peak of New York's coronavirus crisis — when medication, morale and masks were all running low at Brooklyn Hospital Center. Yet sick patients kept coming in, “one after another, after another,” recalls James Gasperino, M.D., the hospital's chair of medicine and chief of critical care.
"I just couldn't believe how many new people were coming in that night, incredibly sick, requiring mechanical ventilation,” he says. “It was overwhelming."
Over time, Gasperino saw the entire hospital transform into a makeshift intensive care unit to accommodate all of the critically ill coronavirus patients. While some were indeed young, the vast majority of those bearing the brunt of COVID-19's wrath were older adults.
More than 1,600 miles away from Brooklyn Hospital Center, Faisal Masud, M.D., has dealt with a similarly dire situation at Houston Methodist Hospital, where he is the director of critical care. Masud describes the COVID-19 patients he's seen as “very complex” and “very, very sick.”
"They needed so much care,” he says. They have also needed emotional support. Similar to Brooklyn Hospital Center, a large share of patients who have received intensive care for COVID-19 at Houston Methodist were 60 or older. And despite being able to connect with their loved ones virtually, they are unable to see or say goodbye to their spouses, children, grandchildren, nieces or nephews in person once they enter the hospital.
"They don't get to hug them. They don't get to hold their hands,” Masud says.
































































More on health
New Federal Rule Makes COVID-19 Vaccines Free
Americans with Medicare, Medicaid and private insurance, as well as uninsured, won't pay10 Days or 14? Understanding COVID-19 Quarantine, Isolation Guidelines
CDC updates recommendations with alternatives to prevent coronavirus spreadIs Pink Eye a Symptom of COVID-19?
Viruses are among the common causes of conjunctivitis