Staying Fit
It’s tempting to heap blame on the owners of America’s nursing homes—to argue that the pursuit of profits led to poor care and so many coronavirus-related deaths.
The reality, however, is more complex.
AARP asked me to explore the business of nursing homes and the culpability of their owners for what has transpired. Clearly most operators reacted to the pandemic as best they could. But what I found was that the industry’s complex and murky financial structure fails to safeguard the health of residents and staff.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
While the overall profits reaped by owners are secret, COVID-19 is clearly hurting nursing homes financially. Fully 55 percent of them claim to be losing money, and 72 percent say they may not be able to sustain operations for another year, according to an August survey by the American Health Care Association and the National Center for Assisted Living.
Even the nation’s largest nursing home chain, Genesis HealthCare, says it’s in jeopardy. Genesis, with 360 facilities in 25 states, said in August there was “substantial doubt” about its ability to survive for the next 12 months.
“If there isn’t more money coming in, many members will face decisions about shrinking the number of beds or even closing their doors,” says Katie Smith Sloan, CEO of LeadingAge, an organization that represents nonprofit nursing homes.
Here is what you need to know to understand the business of nursing homes, and to what extent they caused the mess they are in.


The Industry is Vast
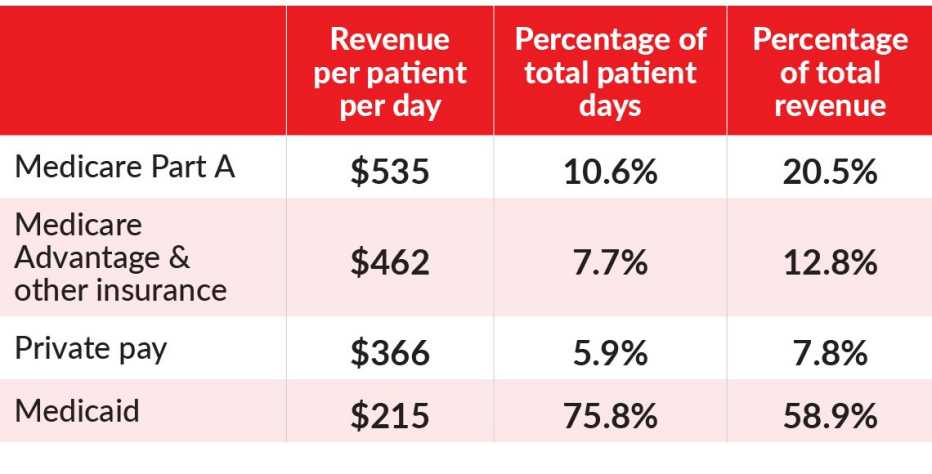
The nation’s 15,600 nursing homes generated about $166 billion in revenue in 2017—a little more than what U.S. hotels took in by renting out their rooms. And nursing homes receive about the same amount for most of their residents as nice hotels get for a night’s stay.
But the similarities end there. For example, roughly 30 percent of nursing homes are owned by nonprofit organizations predominantly affiliated with religious groups, ethnic aid societies and social service agencies. They strive to maximize revenue and efficiency, but any unspent revenue is used to improve and expand their facilities and services.
The remaining 70 percent of homes are for-profit — free to pay out income to owners once they cover operating expenses and other obligations. Owners include national chains, regional chains and stand-alone facilities. About 1 in 7 for-profit homes are controlled by private equity investors — something that can be problematic, as I’ll explain shortly.