AARP Hearing Center

Your liver might be the hardest-working organ in your body.
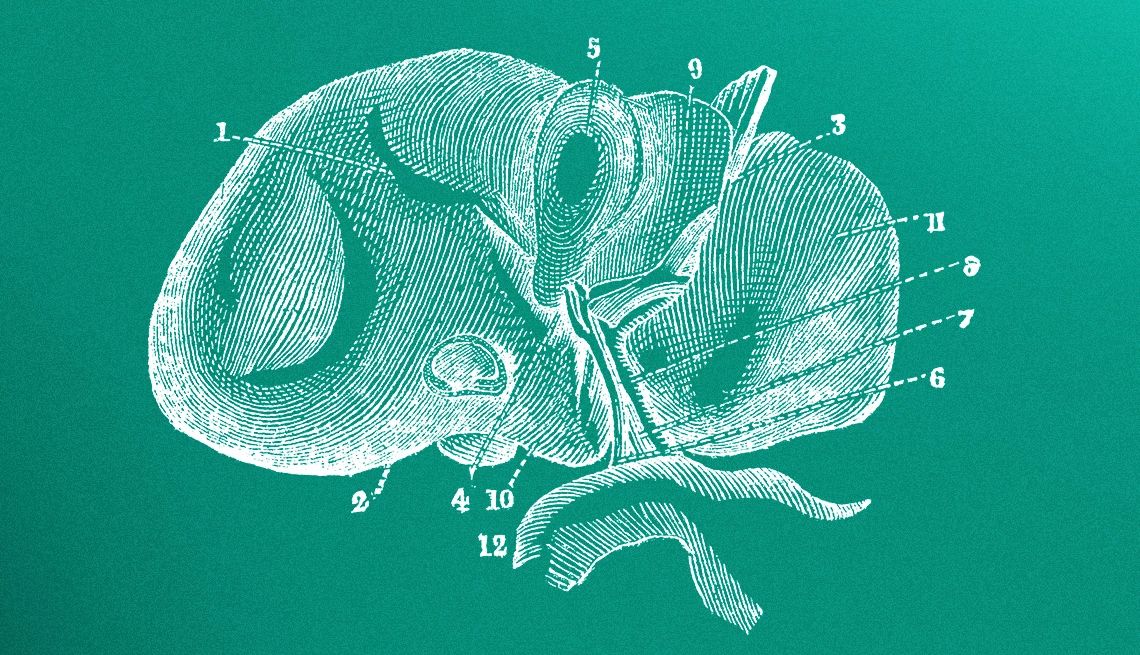
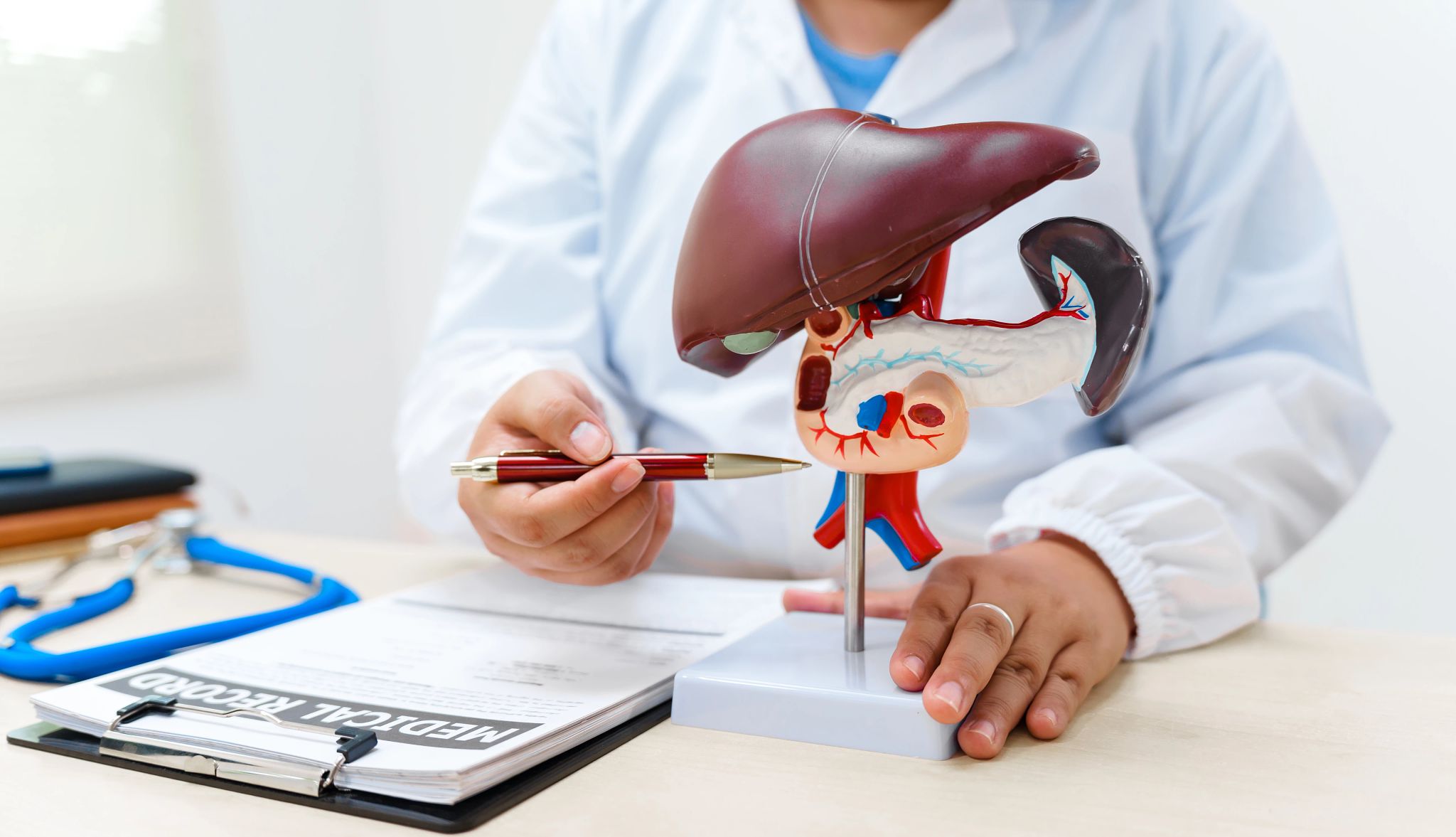
You know that one of its main jobs is to filter out toxins like alcohol from your body. But that’s just one of its more than 500 roles. Weighing about three pounds — with roughly the dimensions of a football — this spongy, reddish-brown organ nestled on the right side of your body under your ribcage works 24/7, helping to fight infections and regulate blood sugar levels, and producing hormones and proteins used throughout your body. And it can regenerate: If part of a healthy liver is surgically removed, the cells divide and begin to regrow tissue within days.
“The liver is incredibly resilient,” says Meena Bansal, M.D., director of translational research at the Division of Liver Diseases at Mount Sinai Health System in New York. “Evolutionarily, it had to be. The liver has to deal with everything we eat and protect the rest of the body. It’s the first line of defense. It is the detoxifier, it’s the cleanser, it’s the metabolizer of any drugs.”
But the liver isn’t immune to the stresses of aging. While we all know that decades of heavy drinking or certain drug use can damage the liver. So, too, can weight gain and an unhealthy diet: An estimated 100 million people in the U.S. have a dangerous buildup of fat in their liver that's known as metabolic dysfunction-associated steatotic liver disease, or MASLD. A study published last year found that nearly 50 percent of people 65 and over have it.
Yet thanks to its superpowers of regeneration, the liver has extraordinary resilience; in many people, liver damage can be treated, sometimes even reversed. To find out how to keep your liver heathy, we reached out to top hepatologists who specialize in diagnosing and managing liver disease. Here is what they said.


KNOW YOUR RISK FACTORS
1. How age affects your liver
By age 65, you’ve already sustained significant liver damage. The aging process can be tough on the liver. With aging, your liver is more susceptible to injury and scarring, also known as fibrosis. Damage tends to be more serious and takes longer to heal in older people, in part because our livers shrink with age: By the time you’re 65, your liver has lost between 20 and 40 percent of its original size, and blood flow has decreased by about 35 percent. “Our bodies are basically machines, and like machines they wear out over time,” says Anna Mae Diehl, M.D., a hepatologist and professor of medicine at Duke University. How quickly your liver wears out depends on how healthy it was to begin with, and how much stress it’s endured over your lifetime.
2. Obesity puts you at risk
The prevalence of fatty liver disease in the U.S. is closely tied to the epidemic of obesity. Being overweight doesn’t mean you automatically get fatty liver disease, but older people tend to be heavier — roughly a third of people 65 and over in the U.S. are obese — and that puts you at risk. If you’re eating too much, the excess calories from a high-fat diet are stored in your liver and interfere with how it functions. According to Diehl, at least 60 percent of women over 65 are overweight, resulting in a 60 to 70 percent chance of having a fatty liver. “If you have diabetes, that goes up to 80 percent,” she says.
But there’s good news: According to Grace Su, M.D., president-elect of the American Association for the Study of Liver Diseases (AASLD), fatty liver damage caused by obesity can often be reversed with weight loss and diet changes. “Not everybody over 50 has liver disease,” Su says. “But it’s a disease that manifests later on because the damage caused by liver diseases accumulates, so you may not see it until someone is older.”
3. Even moderate alcohol use causes damage
If you’re a heavy drinker or even a moderate one, there’s a good chance you have some liver damage or liver disease. When you drink, the liver’s process of metabolizing the alcohol creates byproducts that prompt the liver to make more fat while reducing the amount allowed to exit. As excess fat builds up, it then gets stored in the liver. This stored fat leads to injury of the liver cells, which can lead to scarring and cell turnover, which can increase your risk of cancer. Muscle can absorb extra alcohol as well — which is one reason why men can tolerate booze better than women — but as we get older, we tend to lose muscle mass. That’s why alcohol both affects us more strongly as we age, and causes a greater degree of damage.
According to the Centers for Disease Control and Prevention (CDC), moderate drinking for women is now defined as one drink a day; for men, it’s two. By cutting down on your alcohol consumption or, better yet, quitting, you can halt the progression of liver scarring (called fibrosis), and your liver function may improve, depending on when you stopped drinking.
4. Look at your medications
Although one of your liver’s main jobs is to metabolize medications, some meds can cause drug-induced liver injury (DILI). “Believe it or not, almost any medication makes someone susceptible to develop liver injury. There is no good way to avoid it as we get older,” says Sammy Saab, M.D., medical director of the Pfleger Liver Institute at the University of California Los Angeles (UCLA). And we’re not talking Breaking Bad–style illegal substances. Even high doses of OTC pain relievers such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs); statins used to lower cholesterol; and prescription steroids are potentially harmful to the liver, mostly if you’re taking doses beyond what is recommended on the label.
People with liver damage should limit their daily intake of acetaminophen to 2,000 mg or even less if their liver disease is severe; those who drink alcohol regularly shouldn’t take acetaminophen at all. Some antibiotics, such as erythromycin and amoxicillin/clavulanate (brand name Augmentin), which are prescribed for sinus or urinary tract infections, can also damage the liver. While most of the damage is temporary, in some cases it can lead to more serious liver disease. Read the labels before taking any medications, and talk to your doctor to find out the best dosage for you, especially if you’re taking medications for other health conditions. Don’t be your own pharmacist.
5. Test for hepatitis
Hepatitis is uncontrolled inflammation in the liver caused by viral infections, alcohol or autoimmune disorders. There are five strains of hepatitis, but three — A, B and C — are most common in the U.S. Hepatitis A is highly contagious and generally contracted through tainted water or food contamination (you may recall news of tainted blackberries sold in grocery stores several years ago). But it tends not to be long-term and usually resolves without extensive liver damage. Hepatitis B and C, on the other hand, are spread through contact with bodily fluids — from things like unprotected sex, sharing needles, or poorly sterilized tattoo equipment — and can cause long-term liver damage. While hepatitis testing isn’t routine, your doctor may order a test — it’s done with a simple finger prick — if you have a history of high-risk behavior or are showing symptoms of liver disease. Diabetics are twice as likely to contract hepatitis B as the general population because it can spread by sharing glucose monitoring equipment, which puts older people living in long-term care facilities at a greater risk. Hepatitis C is especially problematic because it’s asymptomatic, and most people don’t know they have the infection. But if it goes untreated, hepatitis C can lead to cirrhosis, liver cancer or liver failure.
6. Environmental toxins hurt older people more
Pesticides, air pollutants and heavy metals can accumulate in the liver; older adults have a harder time filtering them out of the bloodstream. This can lead to inflammation, cell damage and potentially chronic liver diseases. Evidence suggests that exposure to toxins plays a role in liver cancer. While environmental toxins can come in many shapes and forms, using an air purifier in your home is one step you can take to reduce your exposure, especially if you live in an urban area or one with high levels of air pollution.
7. Family history can quadruple your risk
If you have a family history of liver cancer, you’re four times as likely to develop the disease than people without a history. Researchers have found that certain genes may make you more likely to develop fatty liver disease, which may help explain why MASLD is more common in certain racial and ethnic groups. Scientists are still studying the genes that may play a role in this. People with hepatitis B or C infections who also have a family history of liver cancer are at the highest risk of developing liver cancer.








































































You Might Also Like
Smart Guide to Reducing Inflammation
31 ways to tamp down the chronic condition
#1 Belly Fat Exercise
How to relieve back pain, improve posture and balance and make your belly fat healthier
Cut Down on Drinking
A sobriety challenge doesn't just need to be for Dry January