AARP Hearing Center


You trip or bump into doors, walls and furniture more often. Playing catch with your grandkids is a challenge. Navigating crowds without colliding into others is difficult. You struggle to see clearly driving at night.
These are all common signs of peripheral vision loss, also known as tunnel vision, a symptom of many eye diseases and total-body health conditions that affect some older adults. It’s best to catch peripheral vision loss early, yet it’s not uncommon for many people to not even notice it until it’s progressed to a point where it is impacting your daily life. Here’s why it’s so tricky to spot compared with central vision loss and tips to keep your eyes healthy.
What is peripheral vision?
First, it’s important to understand what peripheral vision means.
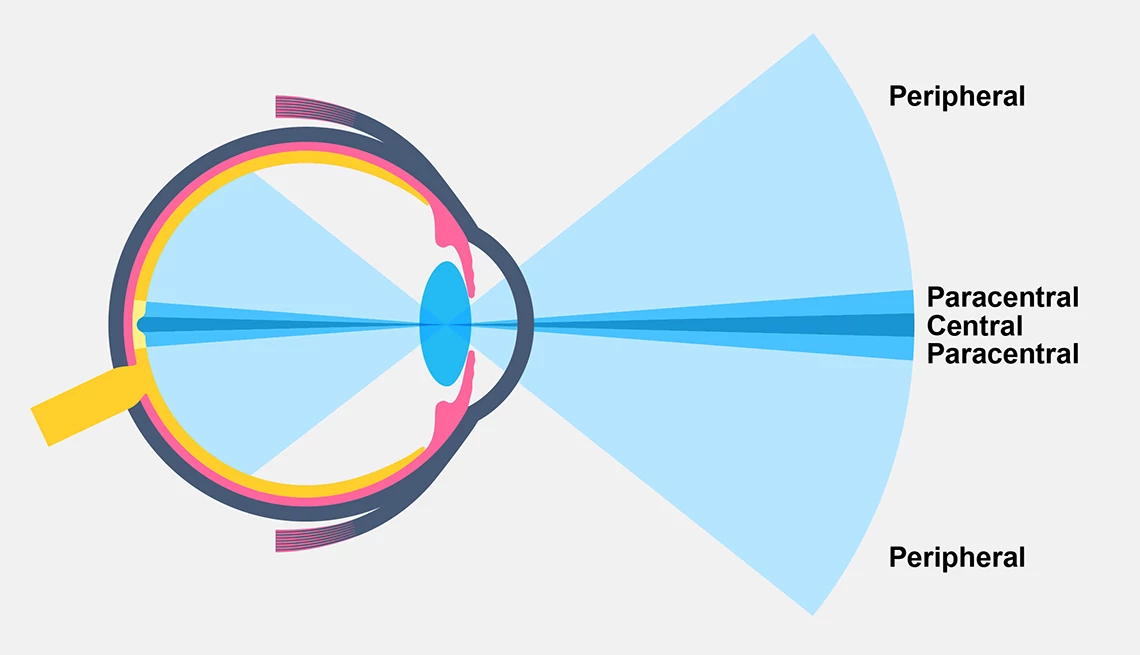
Peripheral vision is seeing off to the right side and off to the left side of your body, or upwards or downwards while looking straight ahead and not turning your head. However, peripheral vision loss can actually affect either the periphery of both eyes together or only one eye. As a result, some older adults think that they have normal peripheral vision because if only one eye is affected, the brain uses information from the other eye to help you see, so they won’t notice it.
Consider that in a 2020 survey conducted by Johnson & Johnson Vision, most adults agreed that healthy vision is linked to quality of life, but only 46 percent of respondents scheduled an annual eye exam. A key reason they skipped their visit? Not noticing any changes to their vision.

What does peripheral vision loss look like?
Numerous diseases and conditions can lead to peripheral vision loss. The condition can be invisible or barely noticeable when a disease is in an early stage, as in the case of glaucoma. If unnoticed, peripheral vision loss can progress to more severe narrowing of the visual field, or it manifests as darkness and blurriness only at the outermost edges of one or both eyes.
As it advances, it can create a type of tunnel vision, as if you are looking through a peephole that keeps getting smaller and smaller. This is part of the reason it makes it harder for people with peripheral vision to drive at night.
Eye exams 101
The American Academy of Ophthalmology recommends that adults get a complete eye examination at age 40 (earlier if you have an eye disease or risk factors such as diabetes, high blood pressure or a family history of eye disease). After that exam, your eye care provider can tell you how often you should have your eyes checked in the future. If you are 65 or older, you should get your eyes checked every year or two, the group says.
Is it normal to lose peripheral vision with age?
Ageing causes the peripheral visual field to narrow between one to three degrees per decade, so it’s impossible for it to remain completely intact later in life. But pronounced peripheral vision loss is not just a normal part of getting older, especially if it’s sudden. Plus, some factors within your control can hurt the eyes, such as inflammation caused by acute or chronic stress and anxiety.
“Believing that you have control over your life and your vision will help you be more proactive about your health and lower your stress,” says Professor Bernhard Sabel, Ph.D. and founder of the world-renowned Savir-Center for vision restoration in Magdeburg, Germany. “Stress can make our vision worse by constricting the muscles around the blood vessels that give neurons in the retina and the brain sufficient energy."








































































More From AARP
Common Eye Conditions in Older Adults
These common symptoms may be signs of an eye disease
What to Know About Eye Floaters
They can be harmless or signal a vision-threatening problem
8 Bad Habits for Your Eyes
Everyday actions that can affect your vision and your healthRecommended for You