AARP Hearing Center

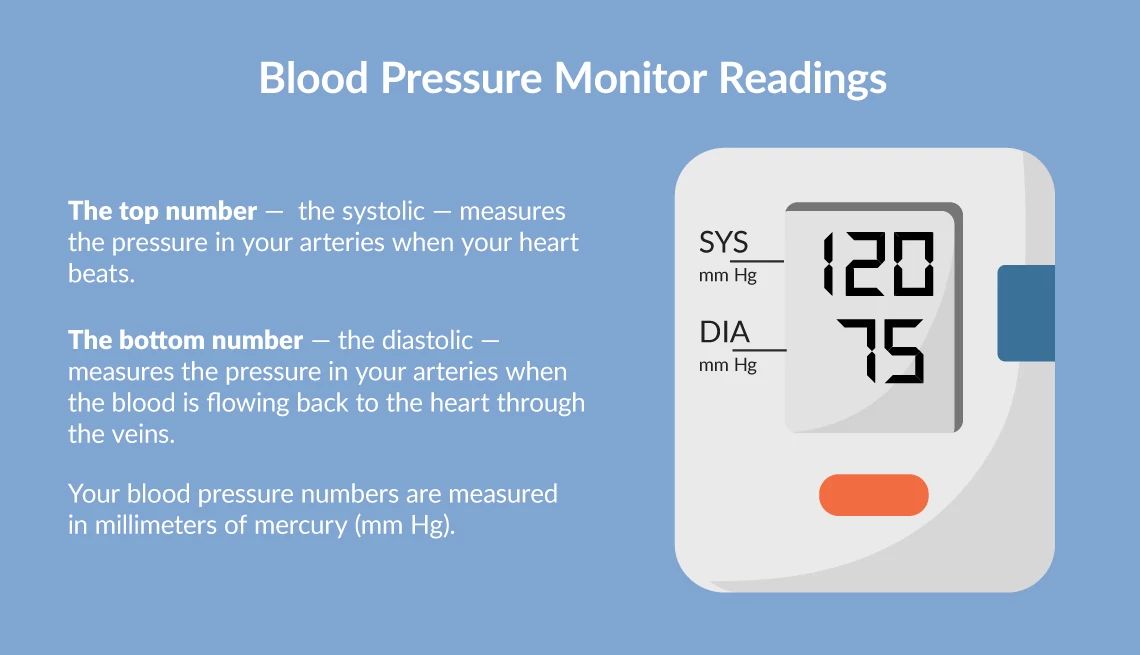
Most of us have had our blood pressure taken at some point and may have a general concept of what are considered “good” or “bad” results. The numerous stages and types of hypertension can seem like a complex maze, yet understanding what risks lie behind the numbers is vitally important, especially for people over age 50.
In 2017, the American College of Cardiology/American Heart Association (AHA) released guidelines defining hypertension as a blood pressure reading of 130/80 mm Hg or higher.
Older people are at particular risk for high blood pressure, because large arteries get stiffer with age and that can cause blood pressure to rise. If the condition isn’t brought under control with medication and lifestyle changes, it can lead to serious medical complications, including heart disease, stroke, kidney disease, eye problems and even cognitive impairment. Under the AHA guidelines, an estimated 46 percent of U.S. adults are categorized as having high blood pressure.
Stages of hypertension
1. Elevated blood pressure
If your systolic pressure is 120–129 mm Hg and your diastolic pressure is less than 80 mm Hg, you are in the elevated range. The primary risk factors for this stage include a sedentary lifestyle, a poor diet and family history. It’s essential to make lifestyle changes to prevent the condition from progressing.
2. Stage 1 hypertension
Systolic pressure of 130–139 mm Hg or diastolic pressure of 80–89 mm Hg indicates stage 1 hypertension. For those over age 50, this stage significantly increases the risk of cardiovascular diseases. Regular monitoring and lifestyle modifications, such as reducing sodium intake and increasing physical activity, are crucial.
For anyone over age 75 — or anyone who smokes or has risk factors for diabetes, kidney disease, high cholesterol or cardiac disease — a blood pressure of 130/80 should be your indicator to start talking to a doctor, says Jordana Cohen, M.D., associate professor of medicine (renal-electrolyte and hypertension) at the Hospital of the University of Pennsylvania. “Under the age of 75 and [with] no other risk factors, 140/90 is when we really start treatment.” However, 130/80 is still considered elevated, and people should think about lifestyle modifications and ways to try to bring their blood pressure down.
“For my patients, I recommend starting medication if their blood pressure reaches stage 1 … and lifestyle changes, including exercise and nutrition adjustments, are not allowing them to reach their goal,” says Benjamin Galper, M.D., a cardiologist at Kaiser Permanente and chief of cardiology of the Northern Virginia service area. “It is especially crucial for individuals over 50 to manage their blood pressure effectively to significantly reduce the risk of heart disease and stroke.”
3. Stage 2 hypertension
People with a confirmed systolic pressure of 140 mm Hg or higher or a diastolic pressure of 90 mm Hg or higher are considered to have stage 2 hypertension. This stage puts them at a high risk for heart attacks, strokes and kidney damage. Immediate and sustained medical interventions, along with lifestyle changes, are necessary to manage this condition.
To get an accurate reading of your blood pressure, Cohen recommends checking back-to-back readings, about 30 seconds to a minute apart, in the morning and in the evening before going to bed, at least an hour after dinner, for a minimum of three days per month. For more detailed directions to checking your blood pressure, see AARP’s guide to high blood pressure symptoms and causes. For stage 2 hypertension, Galper usually prescribes medication right away to bring blood pressure down quickly and prevent complications.

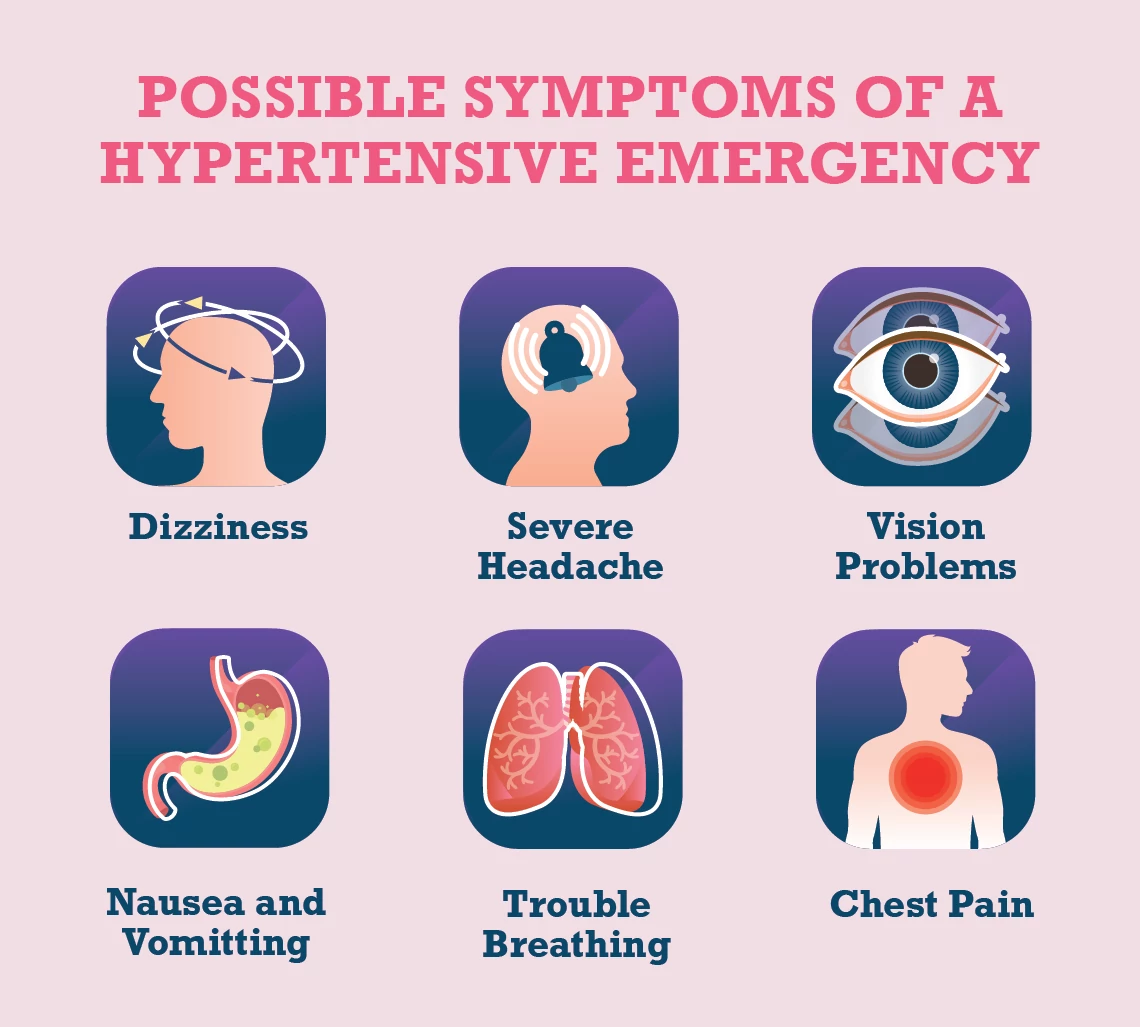
4. Hypertensive emergency and hypertensive urgency
Hypertensive urgency occurs when your blood pressure exceeds 180/120 but you are not experiencing symptoms of damage to a vital organ, such as your heart, brain, kidneys or eyes, Galper says. Cohen refers to this stage as uncontrolled hypertension. If you see these numbers, it’s important to recheck your blood pressure immediately. If it remains high, seek medical attention as soon as possible to adjust your treatment plan and prevent any potential damage.




































































More From AARP
Does Anxiety Raise Your Blood Pressure?
Explore the links between anxiety, stress and blood pressure6 Ways to Lower Your Blood Pressure Without Medication
Try these tactics to help fight hypertension and bring your numbers down
19 Heart-Smart Choices to Make Throughout Your Day
Treat your heart right morning, noon and night with these easy, research-proven, expert-endorsed ideas
Recommended for You