Staying Fit


If you’re a family caregiver who is keeping score — even more than three years since the pandemic walloped the world — the score is still COVID 1, Caregivers 0.
That is the conclusion of AARP’s new comprehensive Long-Term Services and Supports (LTSS) Scorecard, which sprinkles bits of hope along with torrents of recommendations and warns that major gaps in long-term care for older adults persist in all 50 states long since COVID tossed a societal money wrench into the nation’s caregiving system.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
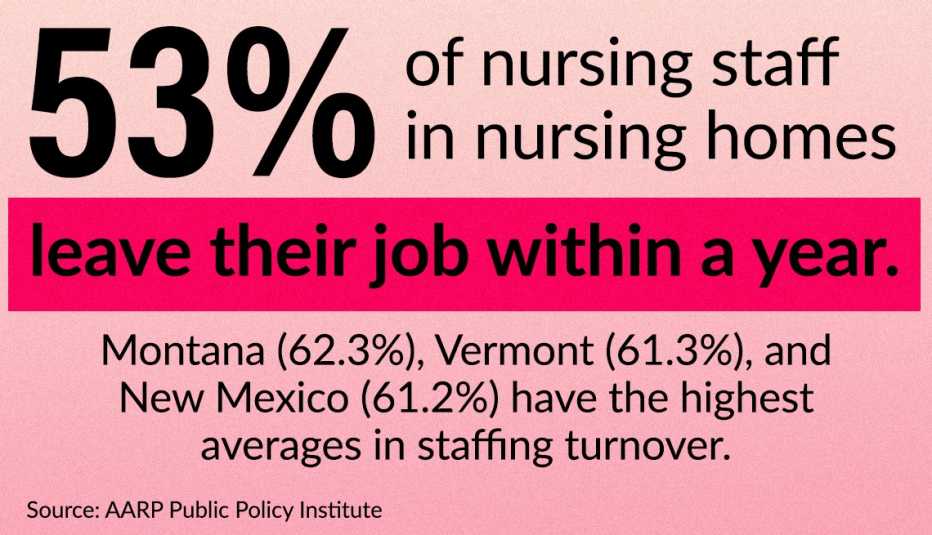
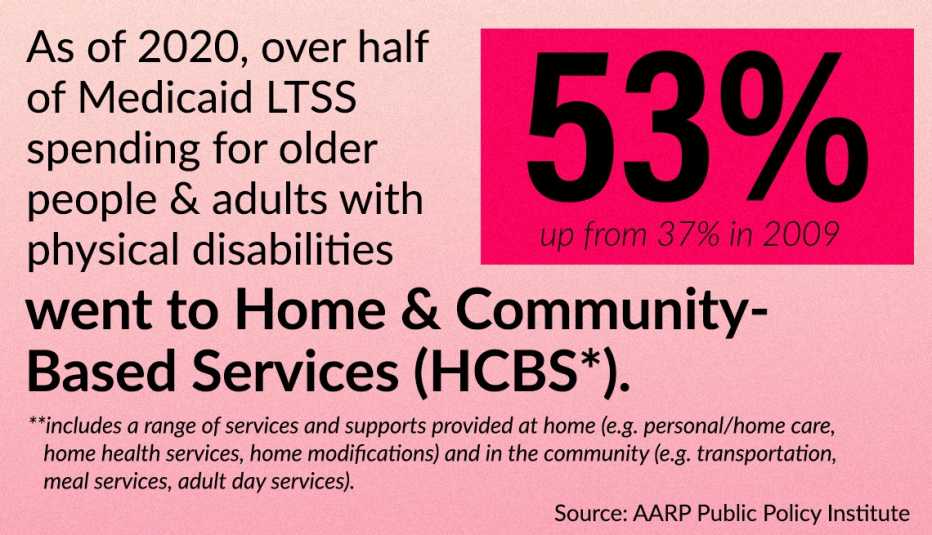
At issue: The long-term care system has mostly failed to rebound even more than three years after COVID-19 began. This is the first LTSS Scorecard that crunches data — using a variety of publicly available sources, such as the Centers for Medicaid and Medicare Services, the Census Bureau’s American Community Survey and the Bureau of Labor Statistics — from the very height of the pandemic and beyond. Even as the cost of home care has greatly increased, the availability and quality of direct care workers have suffered, the report concludes.
“What’s taking so long?” asks Susan Reinhard, the AARP senior vice president who directs its Public Policy Institute. “If COVID hasn’t taught us that you need to support family caregivers, what more do you want to happen?”

Even then, two stalwart states in particular — Minnesota and Washington — and the District of Columbia have continued to innovate with unique ways to support family caregivers at the state level, says the report, which was three years in the making.
The LTSS Scorecard — a charitable project made possible by a grant from AARP Foundation, with support from The SCAN Foundation, The Commonwealth Fund and The John A. Hartford Foundation— has been updated every three years since 2011. It is an innovative mechanism to encourage each of the 50 states to carry its own long-term caregiving weight by ranking the states from best to worst in long-term care services. The data-rich report factors in everything from family care services to the long-term care workforce to equity in nursing homes to emergency preparedness.
Minnesota (ranked first), Washington (second) and the District of Columbia (third) led the way, primarily due to their strong support for family caregivers. South Carolina (ranked 49th), West Virginia (50th) and Alabama (51st) are at the very bottom of the LTSS Scorecard.
Urging all states to improve
States ranked at the very top tend to have very strong leadership both inside government and in the private sector who have made the issue of long-term care reform a priority, Reinhard says. Those ranked near the bottom tend to be laggards in caretaking innovation.
“Long-term care is the stepchild of health care,” Reinhard says. “No one likes to think about it. No one likes to think about being a family caregiver.”




































































More From AARP
A Watchful Eye and a Willing Ear for an Older Adult
Not all aging loved ones need medical help. For some, a care companion could be the right fitCaring For a Loved One at Home
Tips for keeping an older family member comfortable and safe, in their home or yours
Understanding Long-Term Care Insurance
Basics about coverage, premiums and policy options