AARP Hearing Center

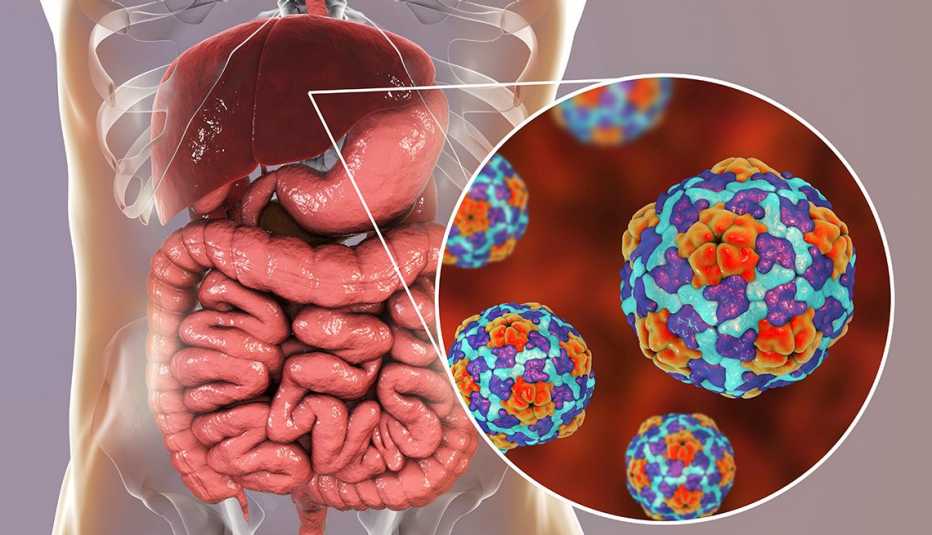
After decades of decline, the number of hepatitis A cases in the U.S. has exploded in recent years, increasing 1,325 percent from 2015 to 2019, according to the Centers for Disease Control and Prevention (CDC).
This highly contagious liver disease can be passed from an infected person or from contaminated food. In recent years there have been hepatitis A outbreaks linked to tainted blackberries sold in grocery stores, imported strawberries used in smoothies at Tropical Smoothie Café locations nationwide and everything from pizza to salads served at major restaurant chains.
Although children are now routinely vaccinated against hepatitis A, most older adults aren't protected, even though they are at higher risk of complications. Only 6.1 percent of adults age 50 and older have received the vaccine, according to the CDC.
Hepatitis A is found in the stool and blood of infected people. It spreads when someone unknowingly ingests even a microscopic amount through food, water or the environment, says Jeff Goad, a pharmacist and public health expert who is vice president of the National Foundation of Infectious Diseases. The illness can also be spread through sexual contact.
In 2019 alone, 31 states reported over 18,846 hepatitis A cases and more than 225 people died from the disease.
Although national numbers for 2020 aren’t yet available, the disease continued to spread in some areas during the COVID-19 pandemic. For instance, North Carolina health officials issued an alert in April 2021 about a marked increase in hepatitis A cases in 2020 and 2021, with more than 60 percent of patients requiring hospitalization.
Much of the spread happens in homeless communities, with outbreaks reported in cities including San Diego, Los Angeles, Miami and Philadelphia, and in Florida and Kentucky.
But the number of foodborne cases has also grown, Goad says, as the United States increasingly relies on imported fruits and vegetables. “For better or worse, our country is very dependent on other countries for our produce, including countries where there are outbreaks,” he says.



































































More on Health
What to Know About the Coronavirus Vaccines
Questions continue as millions of Americans get immunized
Where to Get Your Flu Shot
Most major retailers offering both regular and high-dose vaccinesThese Are the 8 Vaccines You Need After 50
Are you up to date on all the recommended vaccines?