AARP Hearing Center


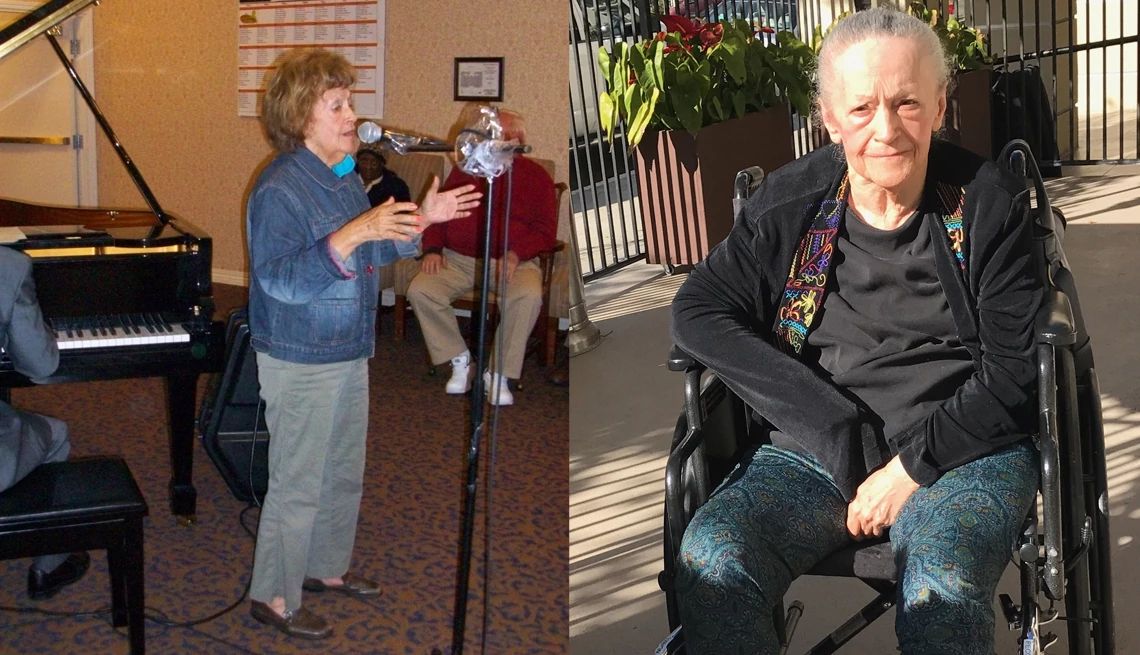
When filmmaker Susie Singer Carter placed her mom in one of Los Angeles’ top-rated assisted living facilities, she believed she was doing everything right. Her mother had Alzheimer’s disease but remained physically strong and socially engaged. But within a few months, her mom, who once held court at the facility every Friday singing songs with a piano player, became unrecognizable: silent, immobile and incontinent. “I thought it was the disease progressing,” Carter recalls. “But it wasn’t. It was actually the drugs.”
That revelation launched Carter on a quest to uncover the hidden epidemic of overmedication that is quietly robbing individuals of alertness, independence and vitality. Her mom had been given the sedating medication Depakote without her knowledge or consent. She found out only when she received a call from her mother’s primary care doctor. They stopped the drug immediately, but the damage persisted. “Once we got her off it, some of her spark came back, but she never walked again. It was like, ‘Oh, hello again, there you are, I was wondering where you went.’ ”
The story is at the heart of No Country for Old People, Carter’s documentary that uncovers the systemic neglect and abuse of older adults, which includes overmedication, especially in long-term care environments. What she discovered, after interviewing many other families, was how common the problem is, whether at long-term care facilities or even at home under a doctor’s care.

Hidden dangers of overmedication
Many older Americans find themselves managing an ever-growing list of prescriptions, over-the-counter remedies and dietary supplements. While medications are essential for treating and preventing a wide range of health conditions, some may do more harm than good. Interactions between medicines, called drug-drug interactions, can pose serious health risks, particularly when it comes to mental health treatments.
A comprehensive 2018 review of 248 studies found that certain drugs commonly prescribed to older adults — including antidepressants, antipsychotics and benzodiazepines to treat anxiety, seizures and sleeplessness — are consistently linked to a higher risk of falls and other adverse effects.
Join Our Fight for Caregivers
Sign up to become part of AARP's online advocacy network and help family caregivers get the support they need.
As people age, their bodies metabolize medications differently, making them more susceptible to side effects such as dizziness, confusion, constipation and impaired balance. “Even small changes in hydration, nutrition or kidney function can turn a routine dose into a serious risk,” says Sean Jeffery, professor of pharmacy practice at the UConn School of Pharmacy in Storrs, Connecticut. “Any new change in condition should first be considered a drug side effect until other causes are ruled out.”
How do you know if your loved one is being overmedicated or experiencing a drug side effect? Jeffery notes several red flags to keep an eye out for, especially when starting a new product or changing the dose:
- Confusion
- Digestive changes
- Drowsiness or fatigue
- Frequent falls or changes in balance
- Increased irritability
- Loss of appetite
- Memory problems
- Nausea
- Sudden mood shifts
Tamara Goulden encourages families to stay vigilant about any medication changes. When her 86-year-old father, Les, was discharged from a hospital and entered a skilled nursing facility in Scottsdale, Arizona, in January 2025, she had hoped it would be a short, restorative stay. Within hours of arrival, Les discovered a serious medication error by scrolling through his patient portal on his mobile phone. The dosage of metoprolol, used to manage his atrial fibrillation (A-fib), was dangerously low. The facility’s staff acknowledged that they couldn’t verify the hospital's discharge instructions from Les’s phone, so Tamara had to retrieve the correct documents from the hospital and deliver them to the facility herself.
What followed was three weeks of near-daily crises: missed updates, staff miscommunication, unnecessary IVs and Goulden battling the system, every turn just to keep her father safe. It left Goulden with the realization that if her father hadn’t been alert enough to catch the mistake, the consequences could have been fatal.




































































More From AARP
Caregiving for Loved Ones With ALS
Ways to provide support for this progressive disease
The Unique Challenges of Dementia Caregiving
Tips on how to manage such often-difficult care
Managing Symptoms at the End of Life
A host of symptoms can come up during the approach to the end of life.