AARP Hearing Center


Breast cancer can be many different things. For some people, it’s a small, contained tumor that can be treated with a single surgery. For others, it’s an odyssey of chemotherapy, surgery, radiation, and other treatments that may take months or, in some cases, continue for life.
So, caring for someone with breast cancer can mean different things, too.
For Keith Hardeman, 69, of Columbia, Missouri, it meant being with wife Shelley, now 59, at virtually every appointment as she went through multiple surgeries, 16 rounds of chemotherapy infusions, 6 weeks of radiation, and six months of chemotherapy pills. That was all part of her initial treatment for stage 3 breast cancer, which ended six years ago. Today, he says, it means dealing with “scanxiety” every six months when Shelley gets tests to see if the cancer has come back (it hasn’t).
For Cathy Jefferson, 59, of Prospect Park, New Jersey, helping her sister Amy Rayfield through her breast cancer, diagnosed in 2020, sometimes meant picking her up and taking her for a long ride to lift her spirits. For Rayfield, 57, of Paterson, New Jersey, it meant being there with hard-won wisdom when Jefferson, too, was diagnosed with breast cancer in 2021.
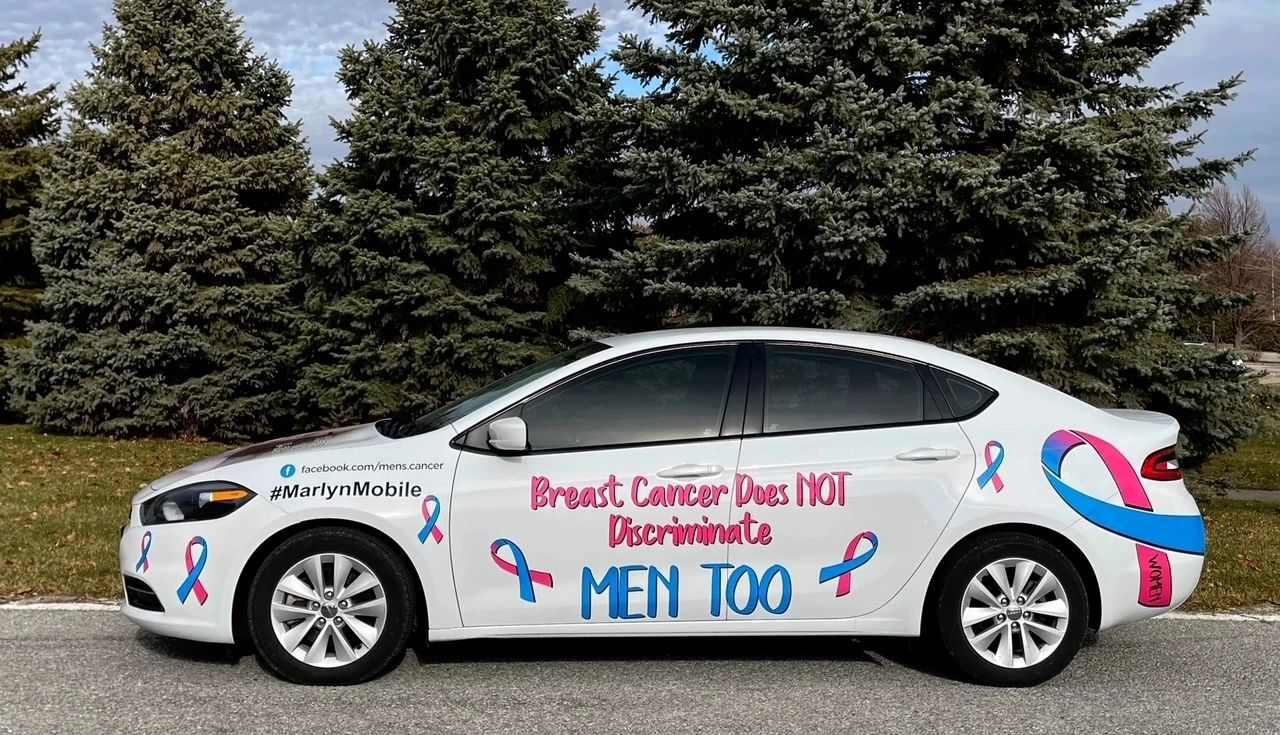
And for Patricia Washburn, 67, of Omaha, Nebraska, it meant helping her husband Marlyn deal with shock — not so much at being a man diagnosed with breast cancer, but at learning that his cancer was too advanced to be cured. His doctors were “hoping to give us five quality years,” but Marlyn lived only five months, she says.
“Every cancer diagnosis and every cancer journey is going to be a little bit different,” says Laura Makaroff, senior vice president of prevention and early detection at the American Cancer Society (ACS).
But, with more than 300,000 cases diagnosed each year and more than 4 million breast cancer survivors in the United States, new patients and their caregivers can draw on a lot of experience. Here’s what to know if someone you care for has breast cancer.


Breast cancer diagnosis and staging
Hardeman says that when a biopsy in late 2017 showed that a lump in Shelley’s right breast was cancer, “we were just immediately in crisis mode.” They urgently wanted to know everything about her diagnosis, treatment options, and likely outcome.
They quickly learned that a complete cancer diagnosis takes time. In their case, it meant waiting a couple of weeks for Shelley to have an MRI and PET scan and for pathologists to examine her biopsy sample further.
Only then, he says, were they able to sit down with Shelley’s oncologist to hear her complete initial diagnosis: A larger-than-expected tumor that had invaded at least five lymph nodes but hadn’t spread further. That made her cancer stage 3 on a scale where stage 0 (called in situ, or non-invasive) is the least advanced and stage 4 is the most advanced.
Breast cancer diagnosis also involves tests to determine whether the tumor responds to the hormones estrogen and progesterone, whether it makes too much of a key protein called HER2, and how abnormal the cancer cells look compared to normal cells. Those factors can affect how the cancer is treated and how difficult it may be to control, according to the cancer society.
Once such tests are done, doctors usually can give people “a reasonable sense of what to expect,” at least for initial phases of treatment, says oncologist Gabrielle Rocque, an assistant professor of medicine at the University of Alabama at Birmingham.


Getting and starting the treatment plan
When someone with breast cancer goes to an oncologist or surgeon to talk about the diagnosis and treatment plan, having a caregiver in the room or listening remotely can be a huge help, says Mari Montesano, an oncology social worker who manages the breast helpline at the nonprofit Susan G. Komen organization. “You don’t hear half the things that are happening in these appointments because you’re so overwhelmed.”
You are hearing “a new language,” says Sarah English, a clinical oncology social worker at Fred Hutchinson Cancer Center, Seattle.





































































)
)


))








More From AARP
Caregiver Guides to Manage a Loved One’s Condition
How can you care for a loved one with dementia, Alzheimer's, diabetes, COPD and other specific diseases?
12 Key Things to Consider Before Caregiving for a Parent
It’s a big undertaking. Make sure you understand all that is involved
10 Common Mistakes That Family Caregivers Make
Experts share how to avoid these caregiving pitfalls