AARP Hearing Center


Chances are, right now, you’re in some sort of pain.
Maybe your back aches, or arthritis is hurting your hands or knee pain is hobbling your walk. Maybe you’re dealing with something even more intense — lingering, life-altering pain from diabetes or cancer.
These are all forms of chronic pain, a type that persists longer than three to six months and rears its ugly head most every day. Chronic pain strikes in many ways — musculoskeletal pain from gout or lingering injuries, inflammatory pain from autoimmune disorders, neuropathic pain from impinged or degenerative nerves, even pain that’s linked to psychological issues. And it hits older adults especially hard.
“As we get older, pain becomes a part of our life,” says Michael Ashburn, M.D., director of pain medicine at Penn Medicine in Philadelphia. With each passing year, the risk of chronic pain grows higher, affecting 26 percent of adults ages 45 to 64 and 31 percent of those 65-plus. Chronic pain does more than deliver unrelenting aches, stiffness and tenderness: It shrinks your life, too. Data from the National Center for Health Statistics finds that more than 1 in 10 adults 65 and older say they have pain that limits their life most days or all the time.
Yet most of the news we’ve gotten about pain management over the past decade has been disappointing, to say the least. Our attempts to treat chronic pain with medication have led to an opioid abuse epidemic so severe that overdoses are now among the leading causes of death for adults ages 50 to 70.
But in the wake of all this despair, there may be real hope. Researchers are discovering new ways to understand our pain and developing novel treatments —including powerful nondrug options — that may help you live more comfortably.
What is pain?
Touch a hot pan or stub your toe, and your body lets you know. Climbing stairs, that telltale crunch makes you slow down.
“Pain is something we experience pretty much on a daily basis, yet it remains a very complex and mysterious phenomenon,” says Haider Warraich, M.D., of Brigham and Women’s Hospital in Boston and author of The Song of Our Scars. “Pain is an alarm bell that goes off in our body to get our attention so that whatever we’re doing to cause the pain is immediately rectified. But one of the biggest mistakes we make is that we think of pain as purely physical sensations.”
It makes sense that your body wants you to take action to stop the pain. Pain turns more complex when it becomes chronic, Warraich says. “Chronic pain is a combination of a physical sensation and an emotion that your body feels,” he says. Meaning, there’s more than just physical damage; it’s emotional, social and psychological too.
“The assumption that what works for acute pain will also work for chronic pain is the root cause of the mistakes we’ve made in medicine and as a society when it comes to the treatment of pain,” Warraich explains. That’s why attempts to throw opioids and other potent drugs at chronic pain conditions have failed spectacularly.
Understanding pain and appreciating its complexity has opened doors for new treatments. And that’s why we’re in such a better place to treat it.

Your brain on pain
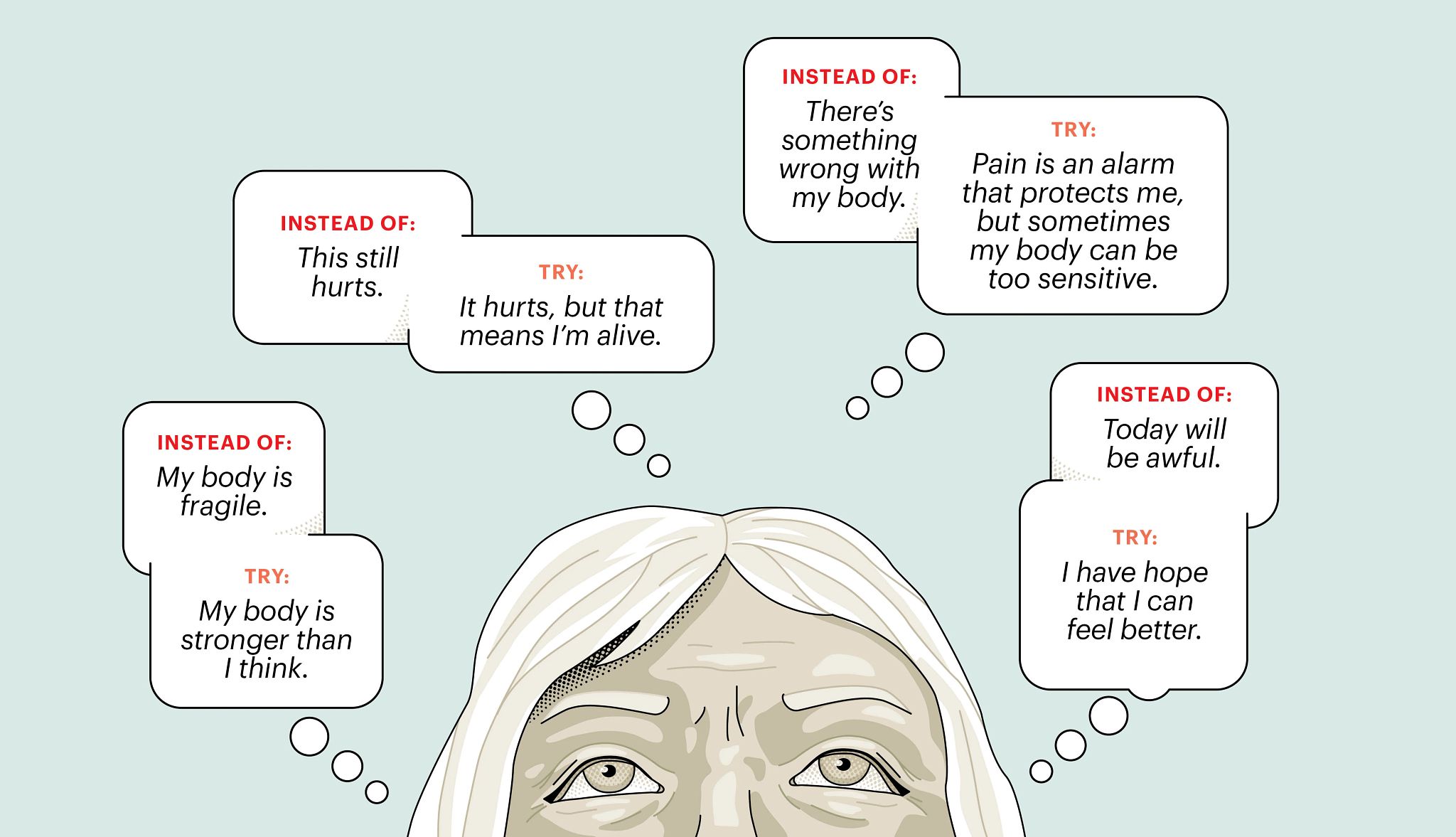
Pain isn’t simply a signal that the body zips to the brain that registers as ouch. That’s an outdated belief, says Tor Wager, distinguished professor of psychological and brain sciences at Dartmouth College in Hanover, New Hampshire. Pain is more of a guess made by your brain in reaction to a physical stimulus: My body is under threat, so what should I be feeling now? “It’s about much more than what’s coming in from your skin and joints. Your brain interprets these sensations in the context of other factors, including your memories, thoughts and feelings,” Wager explains.
When you’re injured, your body becomes hypersensitive to pain. This serves a purpose: You avoid walking on a twisted ankle, for example. As you heal, you gradually move more, and those sensations abate, until you feel normal walking on your ankle again. With chronic pain, however, your attention to these signals becomes amplified, and you can get stuck in a cycle of pain even after your body has healed, Wager says. That doesn’t mean that your pain isn’t real or wasn’t caused by a legitimate injury or illness that kick-started the process. But your body and brain can’t simply transition back, and your nerves remain oversensitive to stimuli, creating lingering pain.
If left to simmer, chronic pain can easily spiral, causing depression and anxiety, sleep deprivation, social isolation, and even economic and financial burden, says Salahadin Abdi, M.D., a pain specialist at the University of Texas MD Anderson Cancer Center in Houston.
The key to pain treatment — and what makes it so tricky — is figuring out what’s contributing to and driving your pain. “For any given person, figuring out the mix of those different things can be complex,” Wager says. It’s not all in your spine or knee joint. And it’s not all in your mind, either. Discovering your personal pain quotient —your tolerance and threshold—is the first step to healing.


















































































You Might Also Like
Save Your Life When Home Alone
From what to do if you have chest pains to what you shouldn’t do if there’s a gas leak, we have tips
Health Risks for People 50+
Research shows the odds of getting cancer and other conditions grow over time; learn how to dodge them
Easy Guide to Painkillers
How different pain medications are used and tips to deal with side effects
AARP Members Edition
Your daily source for candid takes on life, comprehensive guides to living well, tips for saving money, inspiring travel, and more – only for AARP membersRecommended for You