AARP Hearing Center
Monoclonal antibodies have been touted as a highly effective way to keep a mild to moderate case of COVID-19 from progressing into something more severe. But a new study shows that the people who would benefit the most from the treatment — older Americans with chronic health conditions — have been the least likely to receive it.
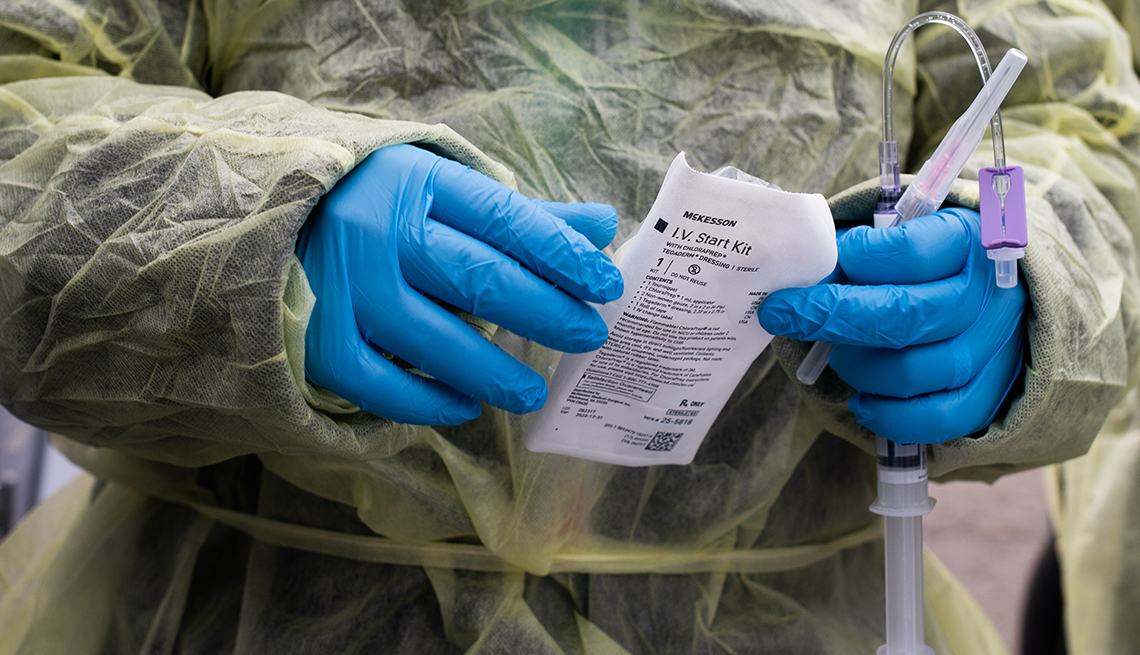
Looking at data from more than 1.9 million Medicare beneficiaries who were diagnosed with COVID-19 between November 2020 and August 2021, a team of researchers found that among those who didn’t succumb to the illness or get hospitalized with it, only 7.2 percent received monoclonal antibodies. These laboratory-made molecules, which are administered intravenously, act as substitute antibodies that help to keep the virus from causing widespread harm after an infection.
Medical Conditions That Increase the Risk of Severe COVID-19
- Cancer
- Chronic kidney disease
- Chronic liver disease
- Chronic lung diseases
- Dementia and other neurological conditions
- Diabetes
- Heart conditions
- Weakened immune system
- Overweight and obesity
This list is not exhaustive but includes many of the chronic conditions that affect older adults.
Source: CDC
What’s more, the likelihood of receiving the treatment was higher among those with fewer chronic conditions. About 23 percent of beneficiaries with zero chronic conditions took monoclonal antibodies, compared with 4.7 percent of beneficiaries with six or more conditions that put them at increased risk for COVID-19 complications. Patients receiving treatment were also less likely to be Black — a population that has been disproportionally affected by COVID-19 disease and death — or dually enrolled in Medicaid. The findings were published Feb. 4 in JAMA.
“Monoclonal antibodies should first go to patients at the highest risk of death from COVID-19, but the opposite happened — the healthiest patients were the most likely to get treatment. Unfortunately, our federal and state system for distributing these drugs has failed our most vulnerable patients,” Michael Barnett, M.D., an assistant professor of health policy and management at the Harvard T.H. Chan School of Public Health and a coauthor of the study, said in a statement.