AARP Hearing Center

When the Food and Drug Administration gave its full approval in July for a new Alzheimer’s drug, there was great buzz among scientists and the media. Alzheimer’s Association CEO Joanna Pike called it “a tremendous step forward.” But while the medication, known as Leqembi, slows mental decline — by about five months in some patients who have early stage disease — it doesn’t repair the damage in the brain or stop the disease from ever progressing. There are also risks involved with its use.
The excitement comes from the fact that finally, after two decades of effort, there’s at least one drug available to slow the disease. It’s been a long slog with many failures along the way to get to this milestone. Researchers have faced a slew of difficulties in coming up with treatments for Alzheimer’s disease, which affects more than 6 million people in the United States, 55 million worldwide, according to the Alzheimer’s Association.
Some of the challenges in developing drugs for Alzheimer’s and other causes of dementia apply to any drug aimed at the human brain. Others are specific to the unique hurdles surrounding Alzheimer’s disease.
1. Scientists aren’t sure what causes Alzheimer’s disease.
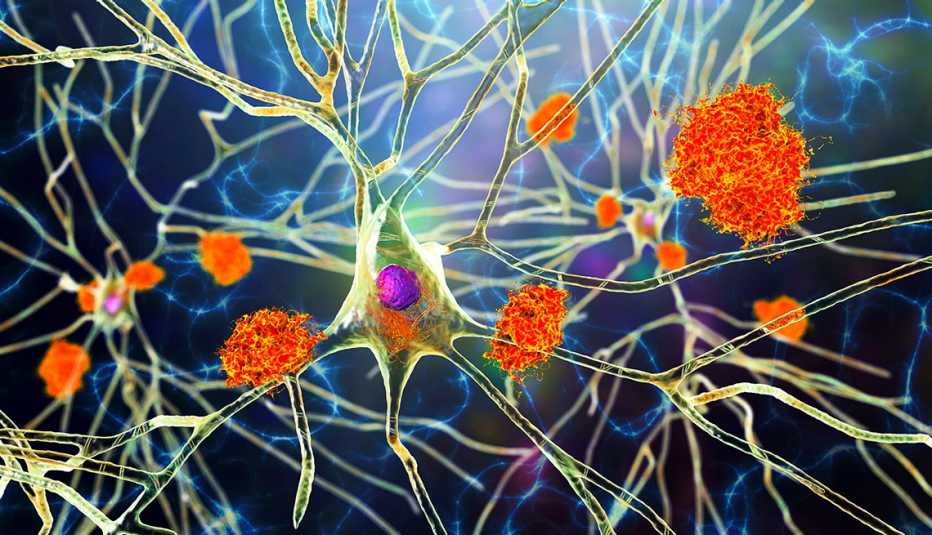
Some firmly believe that Alzheimer’s is primarily caused by what’s known as amyloid plaques. These occur when a protein in the brain breaks down incorrectly into clumps. Those toxic clumps form sticky collections between nerve cells, stopping the cells from functioning as they should. But others are not convinced.
One problem is that the amount of amyloid plaques in a person’s brain doesn’t correspond to whether they show signs of dementia, says neurologist Alberto Espay, M.D., at the University of Cincinnati. By the age of 85, he says, “Sixty percent of us have this in our brains.” Yet many fewer, under a third of people 85 and older, will have dementia, according to the National Institute on Aging.
Another problem: Those antibody drugs, including Leqembi, that clear away amyloid plaques only have small effects on the dementia itself. That’s what makes Lon Schneider, M.D., skeptical. The effects are statistically significant, with patients receiving the drugs showing less decline in cognition than people who got a placebo, says Schneider, who studies Alzheimer’s disease at the University of Southern California Keck School of Medicine. But the size of the difference is so small that many patients and their caregivers might not be able to detect it.
AARP Brain Health Resource Center
Find in-depth journalism and explainers on diseases of the brain — dementia, stroke, Parkinson’s disease, mental-health topics. Learn about healthy habits that support memory and mental skills.
Just because these drugs haven’t shown miraculous effects, the beta amyloid plaques could still be the cause, says psychiatrist Clive Ballard, M.D., who studies cognitive health and dementia at the University of Exeter in England. It may be that the antibody drugs have simply failed so far to clear the right plaques, or clear them from the right places.
2. Most drugs fail during testing.
Getting a new drug from the lab to the pharmacy is a long and costly process. In fact, for all the drugs that make it into human testing, more than 90 percent never get any further, according to the U.S. Congressional Budget Office. The number of drugs for dementia that fail “might be a little bit higher” than average, Ballard says. But “it’s not radically different.” What is different is that there are very few clinical trials for dementia at all. “If you only have 50 trials, you’re touch-and-go whether you’re going to get one compound out of that,” he says. As of January 2023, 141 drugs were being tested in patients for the treatment of Alzheimer’s disease, researchers reported in May 2023 in Translational Research & Clinical Interventions.






































































More From AARP
3 Stress-Reduction Techniques
Try these relaxation methods to ease stress and nourish the body at AARP® Staying Sharp®
What Are the Treatments for Alzheimer's Disease?
Medications help with some symptoms, and new options may slow early stages of this form of dementiaWhat Is Dementia?
It’s an umbrella term for a loss of memory and thinking skills that has various causes, symptoms and treatmentsRecommended for You