AARP Hearing Center

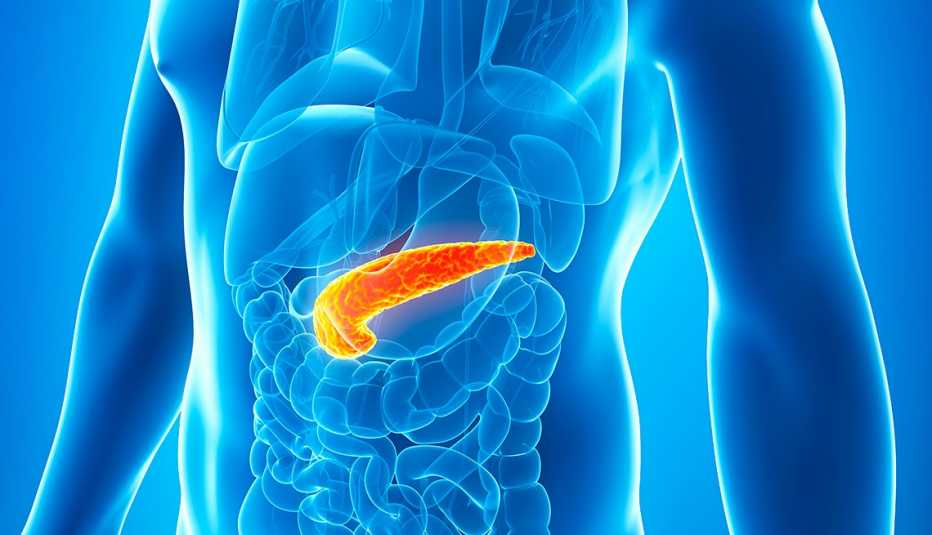
People with diabetes have extra incentives right now to stay on top of their blood sugar levels. Doing so will not only help them live with the disease and avoid complications such as cardiovascular disease and kidney damage but also help them stay safe during the new coronavirus pandemic.
Although diabetics are no likelier to get COVID-19 than the general population, they are far more likely to experience severe complications, even death, if they contract it.
According to a recent report in the Lancet, the risk of death from COVID-19 is up to 50 percent higher in people with diabetes than in those without it. To get a handle on why that is, researchers are looking at the role blood glucose may play.
"It's thought — and this is all very preliminary — that people with uncontrolled blood sugar might be more susceptible to the effects of COVID, partly because of the way the virus gets into our cells,” says Emily Nosova, M.D., a fellow in endocrinology at the Icahn School of Medicine at Mount Sinai in New York City. “Once someone with diabetes is diagnosed with COVID, even if they have mild symptoms and are recovering at home, what we've seen is erratic blood sugar patterns — either dramatic spikes or dramatic drops."



































































More From AARP
Your Lungs, Heart, Brain and More: How Coronavirus Attacks the Body
Understanding the system-wide toll the virus takes — and how to protect yourselfCoronavirus and Older Adults: Your Questions Answered
A CDC official explains why more risk comes with age from COVID-195 Ways to Boost Your Immune System
Science-backed tips for strengthening your immune response quickly and effectively