AARP Hearing Center
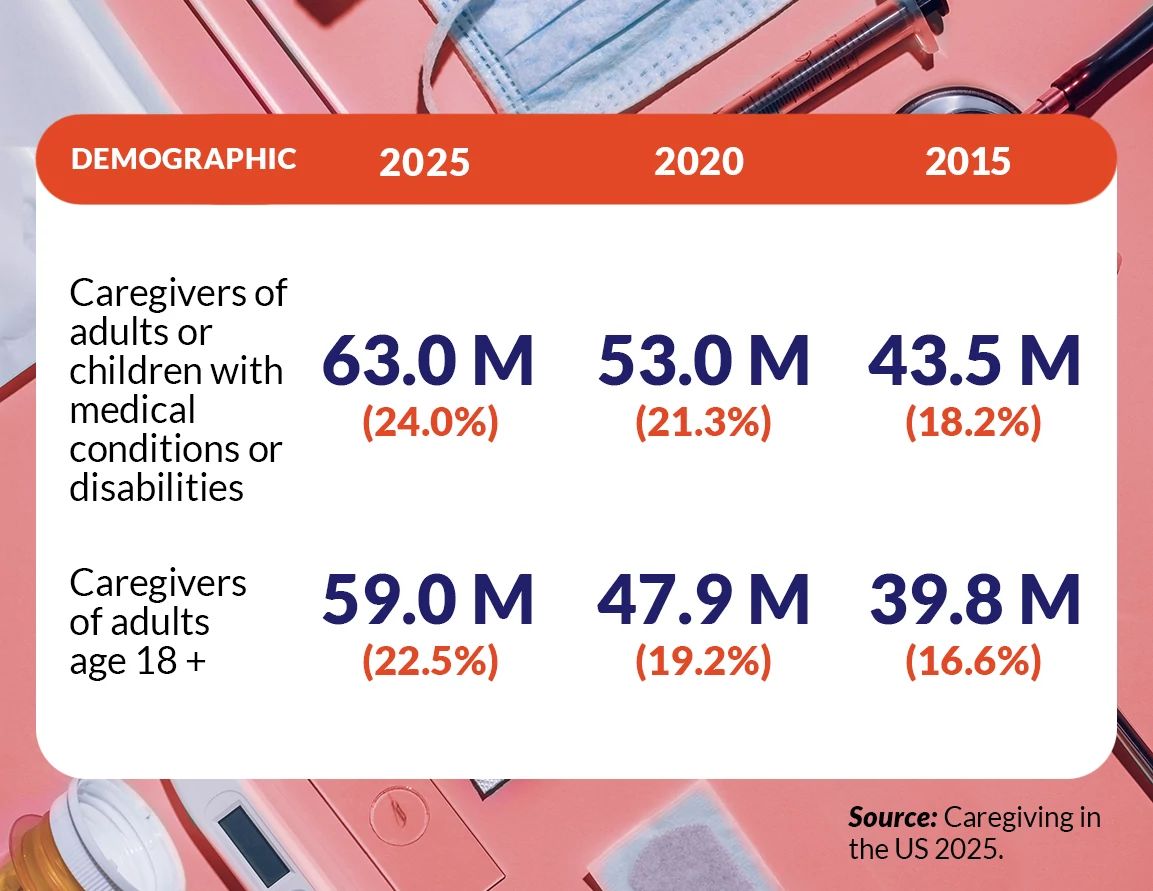
The number of family caregivers has jumped to 63 million Americans, representing a 45 percent increase, or nearly 20 million more caregivers, over the past decade, according to a joint report by AARP and the National Alliance for Caregiving (NAC).
This means roughly 1 in 4 American adults are caregivers, with 59 million caring for adults and 4 million for children under 18 with an illness or disability. The new report, Caregiving in the US 2025, is a near 30-year research series that provides a comprehensive look at the state of caregiving in America, revealing how caregivers are taking on more complex responsibilities, often at the expense of their own health and financial security.
Today’s family caregivers are younger, more diverse and more likely to be juggling multiple roles, with nearly a third caring for both children and adults. Three in 5 caregivers are women, and on average, caregivers are 51 years old. Six in 10 are non-Hispanic white, with 1 in 5 family caregivers living in rural areas.
“When AARP first started tracking caregiving in 1997, the image of a family caregiver was a 48-year-old woman caring for her mother,” says Rita B. Choula, senior director of caregiving at the AARP Public Policy Institute. “We’re seeing growth in younger caregivers, especially among racially and ethnically diverse communities. Now caregivers are just as likely to be a millennial or Gen Z family member, part of the ‘sandwich generation,’ juggling a job, young kids and an aging parent.”

The 2025 report finds that 29 percent of caregivers fall into the sandwich generation category, simultaneously providing care for children and adults. Among caregivers under age 50, that number rises to 47 percent. Many are also managing complex medical tasks that would once have been handled in hospitals by health care providers.
Debbi Harris knows firsthand the complexities of caregiving. The 67-year-old mom of three boys coordinates the care for her 32-year-old son, Joshua, who suffered a brain hemmorage at birth that caused complex medical needs and multiple disabilities including cerebral palsy and hydrocephalus. Joshua depends on a ventilator, tracheostomy and feeding tube to survive. He cannot regulate essential functions like heart rate or body temperature and requires constant, vigilant 24/7 care.


Harris coordinates a round-the-clock operation in their home in Eagan, Minnesota, that rivals a hospital ICU. She handles his bathing, feeding and oral care; monitors for life-threatening complications; and manages his extensive list of medications and appointments.
Her family is her care team. Her husband, Victor, handles night shifts and tracks and orders medical supplies and helps manage Joshua's 24-hour care schedule. Their son Jonathan works full-time to help cover expenses, while eldest son Nicholas regularly fills in on evening shifts and some overnight watches. Harris has also secured nursing benefits through military and state programs, supplementing pay to retain skilled, long-term staff. “Even a subtle change in Joshua’s condition can be the first sign of a crisis,” says Harris. “We vigorously train anyone who cares for him because someone unfamiliar with his complex health needs might miss the warning signs.”






































































More From AARP
Caregivers Get 211 Help in 25 States
AARP expands caregiver support line
Kevin Bacon, Kyra Sedgwick on Love, Caregiving
The couple explores aging and caregiving in their film and in real life
Letting Go of Caregiving Perfection
Caregiving is showing up, not being perfect