AARP Hearing Center
A few hours after getting the second dose of her COVID-19 vaccine one morning in mid-February, Wendy Reiter's arm was a bit sore, just as it was after her first shot. But by evening, she felt flu-like, with body aches, a headache and serious fatigue. “I felt like I was hit by a truck. I was essentially laid up for a day and a half, sleeping on an off all day and feeling out of it,” Reiter, 75, an educational administrator in Westchester County, New York, recalls. “Then the veil lifted, and I felt like my old self again.” Meanwhile, her husband, who is 89, felt fine after getting his second dose. When Reiter asked friends about their experiences, they were “all over the map,” ranging from intense to nonexistent.
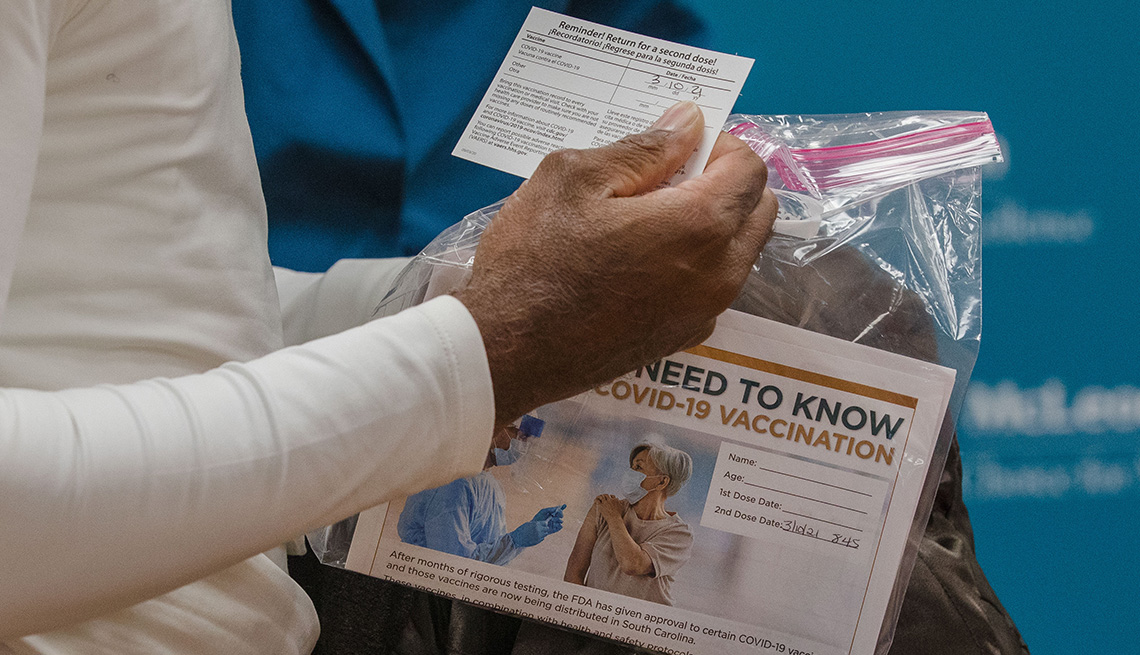
So it goes with the Pfizer and Moderna COVID-19 vaccines. These are reactogenic vaccines, which means they're expected to produce side effects or reactions. Even after the first dose, some people can get local reactions such as soreness or tenderness in the injected arm, or they may feel slightly out of sorts for a day or two, explains William Schaffner, M.D., a professor of preventive medicine and infectious diseases at the Vanderbilt University School of Medicine in Nashville.
Symptoms with the second dose
But the second dose of both vaccines has quickly gained a reputation for packing a punch, with side effects that may include fatigue, chills, headache, muscle aches and pains, and even a fever. “More people — 40 to 50 percent — experience some of these symptoms to one degree or another after the second vaccine,” Schaffner says. This happens because “your immune system is starting to work and cope with the stimulus that comes from the vaccine — so in a sense it's a good thing.”