AARP Hearing Center
By the time you pass 50, staying healthy can sometimes feel like a balancing act. The challenge isn’t just keeping your cholesterol in check or remembering your prescriptions. It’s about managing stress, sleeping well and finding the energy to enjoy life. That’s why so many older adults are turning to integrative medicine (IM), which blends the best of conventional care with evidence-based lifestyle practices.
This isn’t fringe or “alternative” medicine. It’s whole-person care, led by fully trained doctors with an M.D. or a D.O. who’ve earned additional board certification through the American Board of Integrative Medicine (ABOIM) of the American Board of Physician Specialties (ABPS), a credential that signals rigorous training, standards and oversight.
And the interest in integrative medicine is undeniable. In early 2022, the University of Michigan National Poll on Healthy Aging found that two-thirds of adults ages 50 to 80 use at least one integrative strategy — massage, yoga, tai chi, acupuncture or chiropractic care — to boost their mood or ease conditions like pain, insomnia and digestive problems. Ninety-two percent of respondents said those practices were “very” or “somewhat” beneficial, though fewer than 1 in 5 had discussed them with a doctor.
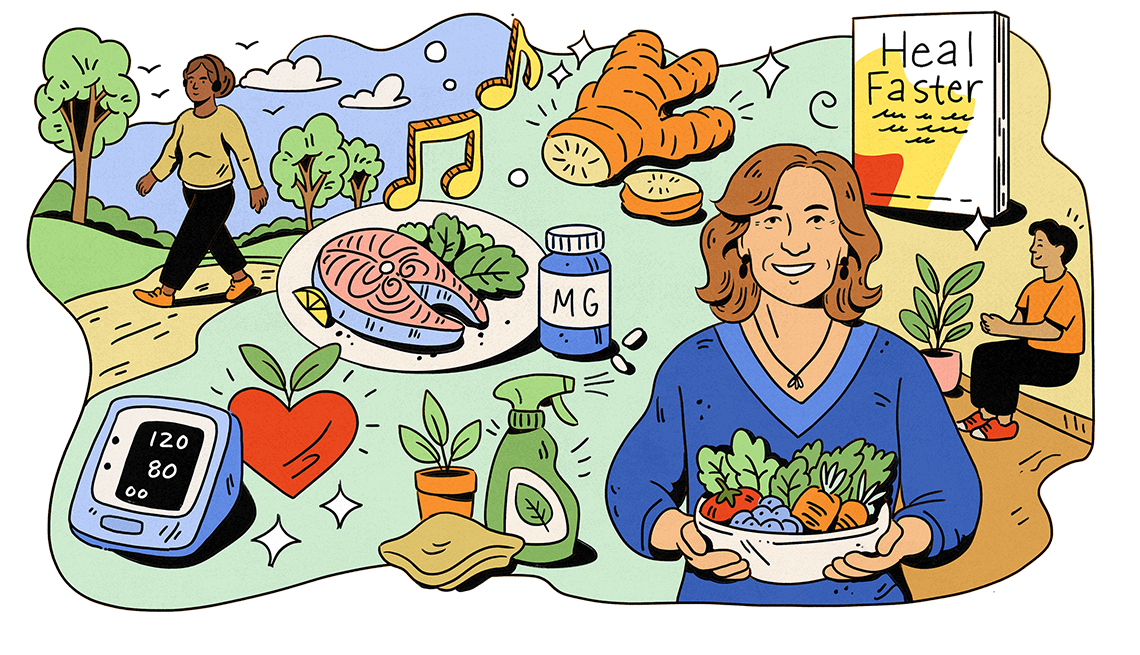
If you’ve been curious about integrative medicine but weren’t sure where (or how) to start, Dr. Victoria Maizes is here to help. She’s the founding executive director of the Andrew Weil Center for Integrative Medicine, a professor of medicine, family medicine and public health at the University of Arizona, and author of Heal Faster: Unlock Your Body’s Rapid Recovery Reflex, written in collaboration with AARP Books and set to publish in January 2026. Maizes has spent her career showing patients how small, integrative shifts can make a lasting difference. Here are 21 tips, in her own words, on how you can make the same commitment to a healthier future.
How to find an integrative medicine doctor


Start by asking your regular doctor if they have integrative training or can recommend someone locally. Then verify credentials: You want an M.D. or a D.O. who’s also board-certified by the aforementioned ABOIM of the ABPS. Many clinicians describe themselves as “double board-certified,” for example, in family (or internal) medicine and integrative medicine. Integrative care should augment, not replace, your standard treatments.
A good IM physician will coordinate plans with your other clinicians (often in the same electronic chart) so that medications, supplements and lifestyle prescriptions don’t conflict. When you interview a candidate, ask whether they provide primary care, consultative care or both; how they share notes with your primary care physician and specialists; how they assess the evidence for supplements; and what visit length, follow-up cadence, costs and insurance options to expect. The Andrew Weil Center for Integrative Medicine also maintains a searchable public directory of fellowship graduates by location and specialty, another solid way to find qualified options.
Insurance may cover your appointments
If you have traditional health insurance (not an HMO), your visits are generally covered if your doctor has integrative training. For HMO members, some plans now bring in integrative doctors as consultants, so check if yours offers that option before assuming you’ll have to pay out of pocket. A little homework up front saves a lot of frustration later and ensures you’re getting advice from someone with the right training, not just a slick website.
Real change starts with your values, not your doctor’s

A big difference between an integrative medical doctor and a traditionally trained PCP is the way we communicate. We teach our physicians a style called motivational interviewing. It’s about understanding your values, because you’re more likely to make changes that align with what you care about.
If a patient smokes, instead of lecturing them about why they should quit, I try to dig deeper into the reasons they cling to the habit. I’ve heard excuses like “It’s the only time I get a break,” “It helps me relax” and “It makes me feel like a rebel.” That tells me the benefit they’re getting from the habit. Then I can ask, “Is there any way it doesn’t serve you?” And maybe they’ll say, “I feel like I’m being a bad role model for my kids.” When the words come from my patient’s own mouth, they carry far more weight than if I just told them what to do.
That’s the power of asking evocative questions. Change sticks when it comes from your own voice and values, not from someone else’s orders.
Expect deeper questions, not just lab work
If you make an appointment with a provider who specializes in integrative medicine, it’s going to feel different than the checkups you’re used to. We don’t just ask about your symptoms, order some tests and write a prescription. We go deeper into your history, asking about topics that may surprise you: your nutrition, your sleep, your stress, your environment, your movement, even your spiritual life. This is all to form a fuller picture of your health and uncover the roots of what may be going on.
Your own habits may hold the cure
When it comes to lifestyle change, the best strategies may be the ones you already know how to do. So one of the first questions I’ll ask is “What’s worked for you in the past?” One person might say, “I committed to my neighbor that I’d walk with her every morning. She’s waiting at 7 a.m., so I have to get up.” Knowing what has worked for you before makes it much easier to create changes you’ll actually stick with. I also like to ask about intuition. Many people have a sense of what they need to do to get well, even if they’ve ignored it for years. They’ll say things like “I need to quit my job” or “I need to spend less time with someone toxic,” or simply, “I need to stop eating dessert.” When the idea comes from you rather than me advising, you’re far more likely to follow through.






































































You Might Also Like
Insider Secrets From a Top Emergency Room Doctor
18 tips to help you get better care and navigate the emergency room with confidence
25 Great Ways to Build Healthy Habits
Cultivate lasting habits with practical, transformative tipsHeart Health Secrets from a Cardiologist
Keep your ticker in great shape as you age