Could Decreasing Inflammation Be the Cure for Everything?
Managing your body's immune response is key to diseases of aging
En español | "Low-grade inflammation.”
It hardly sounds serious at all. An inconvenience, perhaps, like maybe a mild fever or a creaky joint. In the lexicon of aging and disease, there are far more worrisome words: cancer, heart disease, dementia, diabetes. But researchers have suspected for years that all of these health issues, and more, have at their heart one common trigger: low-grade inflammation. And now they may finally have proof.
Cardiologists in Boston have reported on a clinical trial with more than 10,000 patients in 39 countries (mean age: 61) that tested to see if an anti-inflammatory drug could lower rates of heart disease. They discovered that it could. But they also found that the same drug, canakinumab, reduced lung cancer mortality more than 77 percent, and reports of gout and arthritis (conditions linked to inflammation) also fell.
"Inflammation plays a role in everyone's health,” says Dana DiRenzo, a rheumatologist and instructor of medicine at Johns Hopkins University School of Medicine in Baltimore. When inflammation levels increase, so does the risk of disease. But understanding inflammation can be tricky because, when you get a disease, inflammation levels naturally increase as your body fights the condition. Inflammation, in other words, is both good and bad.
Given how crucial this issue is to your health, AARP spoke with some of America's top experts in the field, pored over the latest studies and created this guide to understanding — and overcoming — inflammation.
What exactly is inflammation?
Think about when you catch the flu and your body temperature rises to fight the virus. That's a form of inflammation. So is the redness and swelling that occur when you sprain your ankle; it's the process your body uses to provide the healing chemicals and nutrients needed to help repair the damage.
These are examples of acute inflammation, a temporary, helpful response to an injury or illness. Once the danger goes away, so does the inflammation.
Chronic inflammation, on the other hand, is a slow, creeping condition caused by a misfiring of the immune system that keeps your body in a constant, long-term state of high alert, says Robert H. Shmerling, clinic chief in the department of rheumatology at Beth Israel Deaconess Medical Center in Boston.

It's often the chronic inflammation, not the viruses themselves, that causes much of the damage.
Why is chronic low-grade inflammation a problem?
"Over time, inflammation damages healthy cells,” says Roma Pahwa, a researcher for the National Institutes of Health who specializes in the inflammatory response. Here's why: When cells are in distress, they release chemicals that alert the immune system. White blood cells then flood the scene, where they work to eat up bacteria, viruses, damaged cells and debris from an infection or injury. If the damage is too great, they call in backup cells known as neutrophils, which are the hand grenades of the immune system — they blow up everything in sight, healthy or not. Each neutrophil has a short life span, but in chronic inflammation, they continue to be sent in long after the real threat is gone, causing damage to the healthy tissue that remains. The inflammation can start attacking the linings of your arteries or intestines, the cells in your liver and brain, or the tissues of your muscles and joints. This inflammation-caused cellular damage can trigger diseases like diabetes, cancer, dementia, heart disease, arthritis and depression.
And because it's low grade, “its slow and secret nature makes it hard to diagnose in day-to-day life,” Pahwa says. “You have no idea it's even happening until those conditions show symptoms."
How can something natural to our bodies be so toxic to our health?
"It can be complicated to figure out if inflammation is friend or foe,” Pahwa says. Looking at the four main causes of chronic inflammation, however, sheds some light.
- An outside infection that's hard to kill: You contract a chronic infection like hepatitis C or Lyme disease that lingers in the body for a long time. Your body responds with inflammation that also lingers a long time. In fact, it's often the chronic inflammation, not the viruses themselves, that causes much of the long-term damage related to these diseases.
- Genetics: You inherit a genetic propensity toward a health issue. In some cases, the genes related to these health issues can be turned on by inflammation: Diabetes and cancer are two genetically related diseases that can be triggered by inflammation. In other cases, the gene itself causes a misfiring of the immune system that causes the inflammation in rheumatoid arthritis, multiple sclerosis, lupus and other diseases.
- Environment: Pollution, air and water quality, environmental allergies and a host of other environmental factors can trigger and sustain inflammation.
- Lifestyle: Obesity, unregulated stress, tobacco use, drinking too much, lack of physical activity, lousy sleep and, of course, poor diet are all linked to chronic inflammation.
And getting older increases inflammation, too?
Unfortunately, yes. The older we are, the more exposure we've had to stuff like environmental toxins, stress, alcohol, bad foods and chronic diseases. Plus, aging makes it more difficult for our bodies to properly manage our immune systems, to extract nutrients from food and to shed extra pounds. “There are thousands of articles in the science literature related to aging and inflammation,” says Thomas Buford, an associate professor with the University of Alabama at Birmingham School of Medicine's division of gerontology.
So what makes chronic inflammation happen?
Chronic inflammation is a cascading effect of reactions in the body, Pahwa says. Here's a (very) basic breakdown of what's going on.
- Something triggers the immune system. Whether it's a chronic disease, an autoimmune disorder, weight gain, psychological stress, poor nutrition, exposure to chemicals or allergens — something puts your body in a state of stress and keeps it there.
- The immune system responds. The body goes into attack mode with its inflammatory response, which also includes blood vessel expansion to increase blood flow to the problem areas. Blood is the primary delivery system for all these substances.
- And responds … and responds … and responds. An endless cycle of pro-inflammatory foods, rampant stress, bad sleep and more keeps this process in constant motion because we never give the body a break.
There are “pro-inflammatory foods"?
Yes, and they're the same foods you've been warned about by everyone from your dentist to your cardiologist. (And that's no surprise, because gingivitis and sclerotic arteries are both inflammatory conditions.) Foods high in sugar or high in unhealthy fats (think deli meats and fried foods) are top of the list.
"We don't fully understand it yet,” Buford says, “but now we know our gut microbiome, made up of trillions of bacteria, influences physiologic processes throughout the body.” We're born with a balance between good and bad bacteria in the gut. When that balance is thrown off — known as dysbiosis — it can lead to trouble. “A disregulated microbiome has been associated with metabolic diseases, pulmonary diseases, nervous system conditions, Alzheimer's — and these associations grow as we learn more and more,” Buford says.
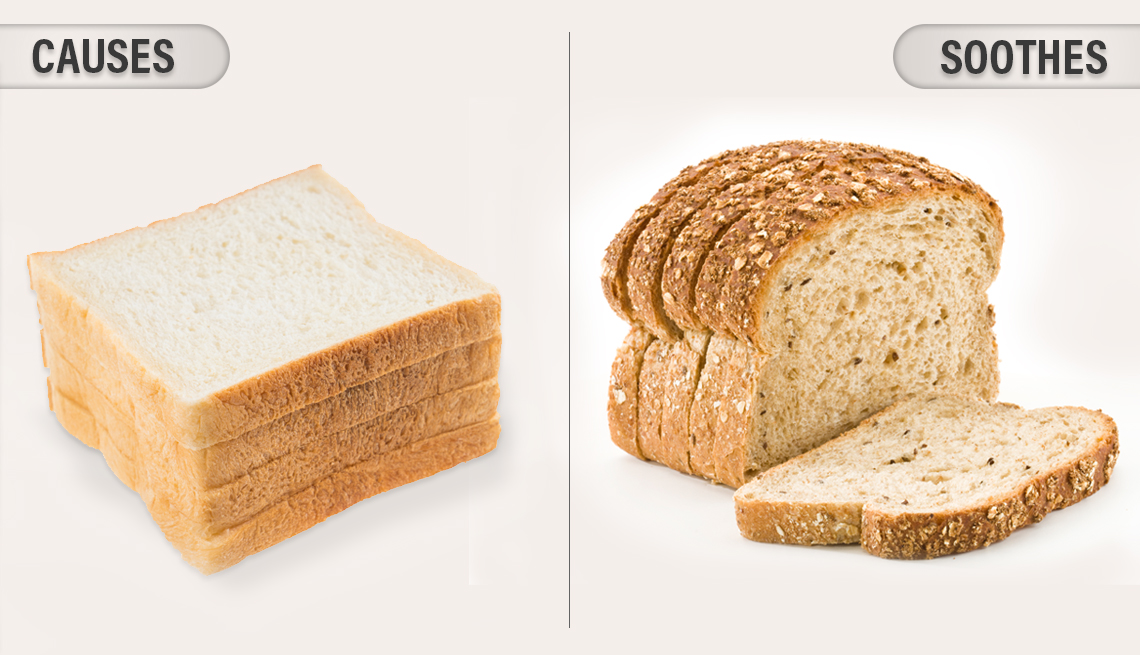
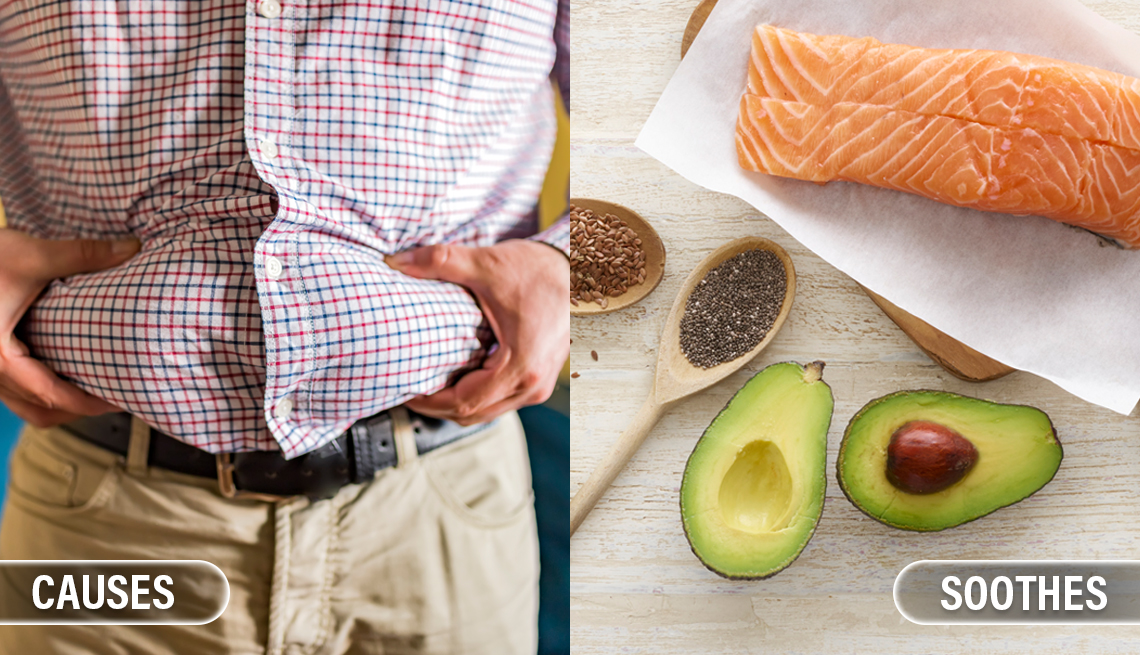
What Causes? What Soothes?
Foods and activities that spark — and help reduce — inflammation
- |
- Photos
We're still learning how these processes work, but one thing we do know is that foods high in sugar and fats, and low in fiber, feed the “unhealthy” bacteria in our digestive tract. When the bad gut bacteria become too numerous, they can damage the lining of the digestive tract. “The intestinal barrier that separates the microorganisms from the rest of your body can become permeable, allowing particles to escape into the body circulation,” Buford says. This is known as leaky gut. The immune system recognizes these particles as foreign invaders and attacks. But since the gut keeps leaking, the immune system keeps attacking, and — boom — you have chronic inflammation. High-fiber foods like whole grains, fruits and vegetables help to restore gut balance.
How do I know if I have chronic inflammation?
First, it's not that you either have it or don't have it. By a certain age, we all have some degree of inflammation in our bodies; the key is to keep it at a flickering ember and not let it erupt into a forest fire. If you smoke, drink a lot, carry a lot of extra weight (especially in your belly), never exercise, eat poorly or constantly feel agitated by stress, your chances of having some level of chronic, elevated inflammation are high. If you are lean, are healthy and lead a balanced lifestyle? You should have less of it. “But it's tricky,” says Shmerling. Inflammation can be measured only by a blood test and interpreted by your doctor.
Did you say that my being overweight is causing inflammation?
Yes, we did. “Fat, especially belly fat, is a highly inflammatory tissue,” DiRenzo says. Every day, your belly fat is creating and releasing inflammatory compounds with Bond-villain names such as interleukin 6 and tumor necrosis factor-alpha. It's why lifestyle factors such as not sleeping well can cause weight gain; it's not just about calories, but about inflammation as well.
Remember, inflammation is a response to cell damage — and fat cells are the body's damsels in distress. They're bloated with triglycerides (a substance similar to diesel fuel) and as a result, they are very fragile and can easily burst and die. When they do, they trigger an inflammatory response as the immune system sends white blood cells to clean up the spilled fuel.
Is there a connection between stress and inflammation?
There sure is. Chronic stress causes an increase in hormones like cortisol and adrenaline, which directly trigger a rise in inflammation. If you have an autoimmunity-based skin condition like psoriasis, you've probably witnessed this phenomenon yourself, says DiRenzo, who often sees it in her autoimmune patients. “They'll say, ‘Oh, I had a big stress week that triggered a flare-up,’ “ DiRenzo says. “And I say, ‘I believe you.’ “
Sounds like I should be asking my doctor to test me for inflammation.
Here's the problem with testing: First, remember that we all have a certain amount of inflammation in our bodies. In fact, our levels fluctuate constantly, so a reading at 8 a.m. will be different from one at 8 p.m. Also, even something harmless like the common cold will spike the levels of disease-fighting chemicals in our blood, DiRenzo says.
Plus, if you're a generally healthy person with no diagnosed issues and you test high for inflammation, what are you going to do about it? For starters: Eat better, reduce stress, exercise more and lose weight. And that's what you should be doing regardless.
That's why doctors don't routinely test for inflammation, DiRenzo says: “Testing should come as a result of certain symptoms like swollen joints.” For example, if you have heart disease, your doctor may test for C-reactive protein (C-RP), an inflammation marker that's been linked to cardiac issues. But just chasing inflammation itself, without specific indicators, can open a Pandora's box of unnecessary testing for patients, DiRenzo says. “Instead of trying to pin down this nebulous term ‘chronic inflammation,’ work closely with your doctor to ID specific-enough symptoms that may lead to a diagnosis of an inflammatory issue."
How about I just take anti-inflammatories like ibuprofen?
Nice try, but no. While researchers continue to experiment with anti-inflammatory drugs, none has been approved for use in fighting chronic low-grade inflammation. “Ibuprofen has side effects such as stomach bleeding and increased blood pressure,” says physician Elizabeth Boham, medical director at the Ultrawellness Center in Lenox, Massachusetts. “There are much more effective ways to address chronic inflammation."
I assume that would be lifestyle changes.
Bingo. Lifestyle is the thing you can change fastest and the one thing you can control. The easy steps are to stay up to date on your vaccinations and wash your hands regularly, because infections trigger inflammation, Shmerling says. Beyond that, food, exercise, sleep and stress relief are the big four.
The antioxidants in fruits and vegetables help to mitigate the cellular damage created by inflammation.
I already eat my veggies.
Brilliant. From an anti-inflammatory food perspective, eating a wide variety of colorful fruits and vegetables is about as good as it gets, because the antioxidants found in fruits and vegetables help to mitigate the cellular damage created by inflammation. Cutting down on pro-inflammatory foods like processed flour, sugar and anything high in fat will also help, even if you can't stand the sight of cauliflower, DiRenzo says.
What else should I eat?
If all else fails, fiber. High-fiber foods feed the good microbes in your gut during digestion, helping to correct dysbiosis. “There's a lot of evidence that a high-fiber diet provides a positive balance of microbes and can potentially down-regulate inflammation,” Buford says. Also important: Avoid unhealthy fats because, he says, “even one high-fat meal can change the microenvironment."
So, less bacon, more broccoli. Is a vegetarian diet the answer?
Nope, unless that's what you want to do. It's true, plant-based foods pack the strongest anti-inflammatory punch. It's also true that red and processed meats can cause inflammation, but you don't have to banish meats from your diet, Boham says. This is particularly important for older adults because protein consumption may help prevent age-related muscle loss. “I recommend a balance between plant — nuts, seeds, beans, grains — and animal protein,” she says. She recommends organic, grass-fed meats and wild-caught fish, which have a lower inflammation factor because they feed on plants and animals that are high in phytonutrients. Try to eat one food from every color of the rainbow every day.
I'm not much of an exerciser. How problematic is that?
Well, research has shown that you don't have to be a marathoner to lower inflammation. In fact, a University of California, San Diego, study found that just 20 minutes of moderate exercise suppressed the inflammatory response. One reason, Buford says, is that exercise can positively affect your gut health (yes, that again). Maybe DiRenzo puts it best: “The difference between someone feeling OK and feeling great is exercise."
But exercise to me is unpleasant and uncomfortable.
So is heart surgery. Which would you prefer? Ultimately, the anti-inflammatory benefits of exercise are worth the temporary discomfort. Even if you have physical limitations — bad knees, for example — exercise will most likely improve them. To get started, DiRenzo suggests picking an activity you can do for five minutes a day. Next week, do it for seven minutes. It could be as simple as a brisk walk. “Yeah, you're gonna be sore,” she says, “but this is a good sore. Build and build and you will start to feel better."
If I'm going to be sore, doesn't that mean my muscles and joints have more inflammation?
Sore muscles would be acute inflammation that'll go away in a day or two. (Good try, though.)
You make it sound like wholesale lifestyle changes are easy. They're not, you know.
True. But isn't attacking one enemy — inflammation — a lot easier than worrying about dozens of them? Here's an idea: If you have to pick one lifestyle area to improve, focus on sleep, both the quantity and quality. It not only lowers your inflammation levels, it also helps you do everything else better. “I find when people give their body time to rest and lower stress, they have an easier time making smart food choices and getting exercise the next day,” Boham says.
Mike Zimmerman is the author of more than a dozen health books, including The 14-Day Anti-Inflammatory Diet.
Video: The Best Foods to Fight Inflammation
More on Inflammation
Editor's note: This article was originally published on November 1, 2019. It has been updated with the AARP Top Tips video.