Staying Fit


Jim Furneaux, 79, was diagnosed with stage 4 melanoma in 2021 after a scan showed the cancer was in his lungs.
Although stage 4 melanoma is the deadliest form of skin cancer, Furneaux is optimistic because his doctors are using a new weapon to fight his disease: a personalized cancer vaccine formulated to attack his specific cancer cells.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
“I was really taken by the technology,” says Furneaux, of Newburyport, Massachusetts. “You have a weapon that is going against your known enemy. It can go right directly to your cells and kill them.”
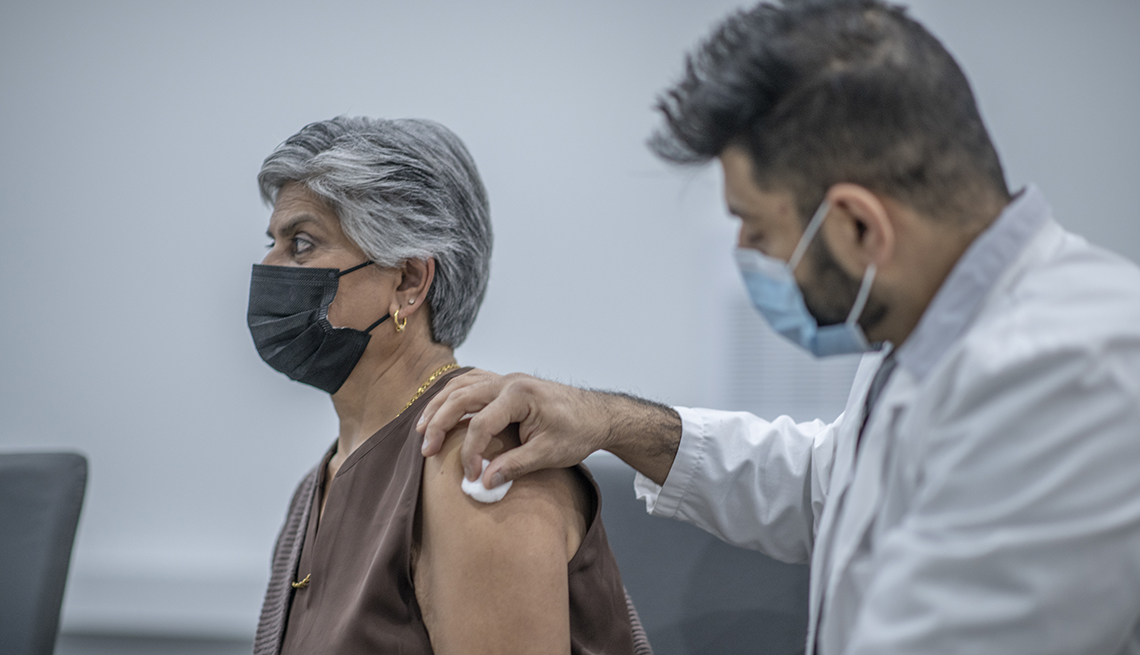
The vaccine, part of a clinical trial at the Dana-Farber Cancer Institute in Boston, is one of dozens being developed and tested across the county to fight different types of cancer.
Not just prevention: Vaccines may help with cancer treatment
When most people think about vaccines, they think about shots that can prevent a disease from developing in the first place, as is the case with the measles vaccine or the flu shot. And already there are two preventive cancer vaccines: the HPV vaccine, which targets a virus linked to cervical cancer, and the hepatitis B vaccine, which helps guard against liver cancer caused by a hepatitis B infection.
But researchers are also studying vaccines as a way to treat cancer once it has already occurred or to prevent it from coming back. Just as vaccines train the body’s immune system to recognize and attack a virus or other foreign invader, scientists have figured out a way to teach it to do the same with cancer cells. And that’s a big deal, because tumor cells are derived from human cells, which makes it difficult for the body to distinguish the good guys from the bad.
After decades of setbacks, researchers say this idea is at a watershed moment. Scientists have discovered new ways to target certain proteins, called antigens, on the surface of tumor cells, and some experts predict that at least some cancer vaccines will be commercially available in the next five to 10 years.
“It’s exciting, because people in the field have thought about this since the 1980s, and nobody could make it happen,” says Patrick Ott, M.D., clinical director of the Melanoma Disease Center at the Dana-Farber Cancer Institute.
One thing to note, however: The cancer vaccines being developed aren’t mass-produced shots for everyone like the COVID-19 vaccine or flu vaccine. Instead, they are formulated for specific patients or groups of patients — either those who have already been diagnosed with cancer, cancer survivors or those who are at high genetic risk.
A vaccine tailored for one patient at a time
The cancer vaccines that have gotten the most attention recently are personalized vaccines, like the one Furneaux received. They are created for a specific person based on the genetic mutations in their tumor cells.
“Every patient has a different tumor with different mutations,” Ott says. To create a personalized vaccine, those mutations are programmed into a vaccine made specifically for that person. The whole process can take six to eight weeks, and experts say it likely comes with a high price tag.















































































More on Vaccines
5 Things to Know About the New COVID-19 Vaccines
Who’s eligible for shots, what they cost, when to get one and moreWhat to Know About the Tdap Vaccine
Details on what the shot does — and when you need it3 Shots This Fall: What to Know About COVID, RSV and Flu Vaccines
Advice on when — and how often — to get them