Staying Fit
I was sitting at the dining room table in the place that had been Dad’s since I was a little girl. On the outside, I was calmly listening to the nurse and matter-of-factly filling out detailed forms. But, on the inside, I was struggling.
I felt the weight of making a huge decision as Dad’s primary caregiver: It was time for hospice care for my beloved father.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
As I took a break from the needed paperwork, my eyes were drawn to Daddy’s bronzed baby shoe, displayed on a nearby cabinet. The shoe was the symbol of life’s start; the hospice forms were signaling an end. The circle of a 94-year life was coming to a close. My heart crumbled.
A person is admitted to hospice care due to a specified health condition, and treatment for that condition stops upon admission because hospice care is not curative care — it’s comfort care. Dad took a medication to help with his Alzheimer’s disease symptoms (but that would not cure the disease; there is no cure), and hospice rules said he would have to stop it, which would have made him much more uncomfortable and more difficult to care for.
Dad also had advancing congestive heart failure that qualified him for hospice. So he was admitted under that diagnosis, and none of his dementia medications needed to be stopped.
Although hospice care is targeted for people who have less than six months to live, I honestly didn’t believe Dad would die that soon. I just couldn’t fathom that after caring for him for more than a decade. But I knew the program would help meet his needs.
And I also knew it would provide more support for my sisters and me as we struggled to care for him while dealing with our own fears and grief. We knew he would die at home, and we wanted to be as prepared as possible. Little did I know he would only live four more months, and hospice would be a critical support.
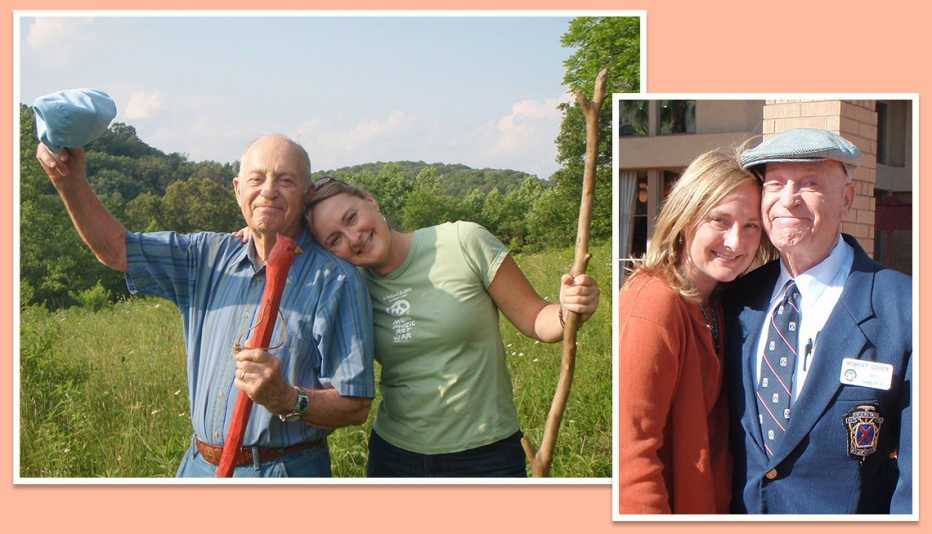
Making the decision
A few months before Dad entered hospice care, as my nephew and I settled him in his recliner after a short walk, I leaned down to give him a hug and a kiss. I asked if he was OK. “Yes, my daughter,” he said in a loud and clear voice, as if to proudly acknowledge that he knew exactly who I was. My heart nearly burst with joy! It had been a long time since he had expressed knowing me so distinctly. Clearly, he felt safe, loved and surrounded by his people. We wanted him to feel that way throughout his final days.