AARP Hearing Center

If you live long enough, you’ll probably get cataracts, an inevitable consequence of getting older. Beginning around age 40, the eye lens can begin to cloud, but you typically don’t notice a change until after 60. By 80, more than half of all Americans will either have cataracts or have had cataract surgery.
“I liken cataracts to wrinkles and gray hair,” says Anupama Horne, M.D., an ophthalmologist and eye surgeon at Duke University in Durham, N.C. “In the end, nearly everyone will develop them.”
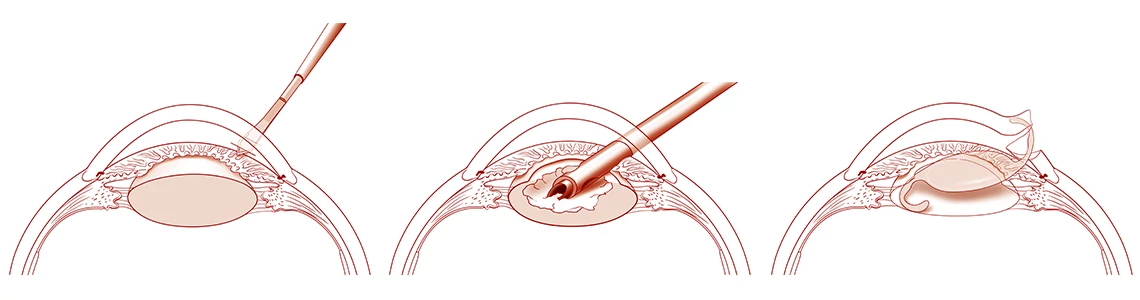
But the good news is that today’s high-tech procedures restore clear vision in about 97 percent of the close to 4 million Americans who undergo cataract surgery every year.


What happens in the eye when you have a cataract?
Imagine a broken lens on a camera. “No matter how much you try to focus the camera, if the lens is broken, you’ll get a blurry picture,” says John Bartlett, M.D., an ophthalmologist and eye surgeon at UCLA Stein Eye Institute in Los Angeles.
Cataracts occur when proteins in the lens of the eye break down, causing the normally clear lens to become cloudy.


The lens in your eye works like a camera lens, focusing light onto the retina at the back of the eye. The retina then sends nerve signals to the brain, allowing you to see clearly both up close and far away. Over time, as we age, proteins in the lens to clump together, clouding the lens. This cloudiness, known as a cataract, gradually makes it harder to see as it grows larger and thicker. Cataracts usually develop slowly and can affect one or both eyes. Unlike infections, they don’t spread from one eye to the other.
What causes cataracts?
Aging is the most common cause of cataracts, but other culprits can contribute, including certain medications, chronic illnesses such as diabetes and cardiovascular disease, and poor lifestyle habits, like smoking or exposure to too much ultraviolet light from the sun. Family history also plays a role.
Because age-related cataracts generally develop over time, worsening vision may not be noticeable in the very early stages. But as the clear lens of the eye slowly turns a yellowish/brownish color, the increased tinting may make it more difficult to read and colors seem faded. Other symptoms include blurry or double vision, glare — when headlights, lamps or sunlight appear blindingly bright — and poor night vision that can make driving hazardous.
“It’s like a piece of clear plastic becomes yellowed and discolored,” says Bartlett. “As new layers are added, it becomes denser and harder.”
Three types of cataracts
Like an onion, the lens is composed of multiple layers. The outermost is known as the capsule. The layer inside the capsule is called the cortex. And the innermost layer is the nucleus. The three types of cataracts are named for their location in the lens:
- Posterior capsular: Unlike the other two, this type of cataract, found in the back outer layer of the lens, tends to develop rapidly.
- Cortical: Located in the outer layer of the lens surrounding the nucleus. Picture a wedge or a spoke — that’s what a cortical cataract looks like to your eye doctor.
- Nuclear: As the name suggests, this type of cataract is found in the innermost layer at the center of the lens. The nucleus tends to darken with age, changing from clear to yellow and sometimes brow



































































More From AARP
Common Eye Conditions in Older Adults
These common symptoms may be signs of an eye disease
6 Best Vitamins for Eye Health
Find out which nutrients are essential for protecting vision
How to Protect Your Vision
21 ways to take charge of your eye healthRecommended for You