AARP Hearing Center

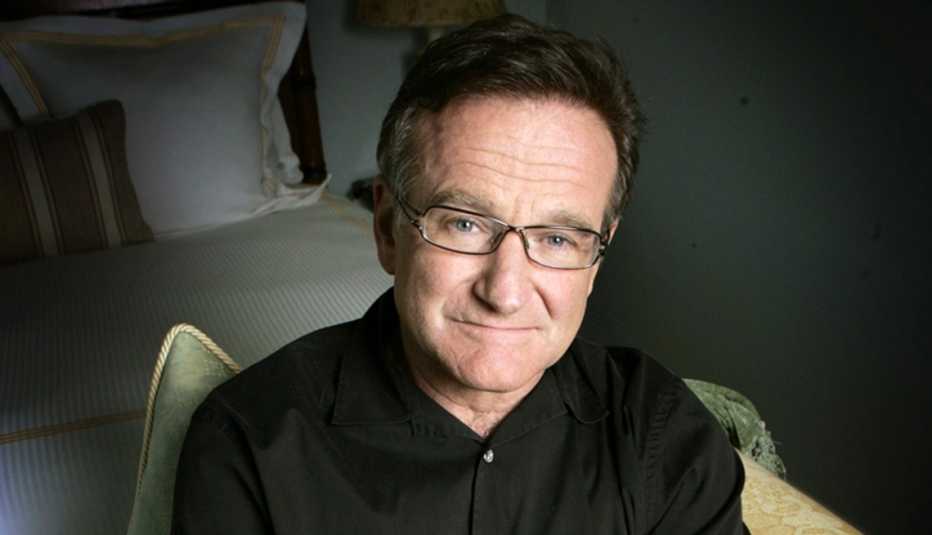
More than 1.4 million Americans have Lewy body dementia (LBD), the second-most common form of progressive dementia after Alzheimer's disease. It struck mogul Ted Turner, actresses Dina Merrill and Estelle Geddes, DJ Casey Kasem, and actor Robin Williams, whose widow Susan Schneider Williams says his last wish was this: “I want to help people be less afraid."
Williams was afraid because he never knew what disease he had. His widow fulfills his last request in a moving, enlightening new documentary about his illness, Robin's Wish, available to stream on Amazon Prime. “During the last year of his life, Robin was confronted with anxiety, paranoia, insomnia, scary altered realities and a roller coaster of hope and despair,” she says. “It wasn't until after Robin's passing, in autopsy, that the source of his terror was revealed: He had diffuse Lewy body disease."
The hidden threats of Lewy body dementia
"Robin struggled with getting the right diagnosis,” says Norma Loeb, who founded the Lewy Body Dementia Resource Center after her mother got the disease; she also consulted on Robin's Wish. “That parallels the experience we hear from people with LBD and their loved ones who call our helpline."
LBD, which generally affects people over 60, is tricky to diagnose because its multiple symptoms resemble those attributed to other diseases. “Susan [Williams] compares LBD to ‘whack-a-mole,’ because symptoms pop up and disappear,” says Loeb. Without knowing why, Robin Williams had mysterious sleep disturbances, thrashing while dreaming. He also experienced a sudden onslaught of memory issues. “When Robin was doing Night at the Museum III, he couldn't remember his very few lines,” says Loeb. “And he had just done Broadway twice a day with hundreds and hundreds of lines and didn't make a single mistake. He thought, ‘What the heck is going on?'"
For Loeb, her mother's LBD first manifested in her having trouble balancing her checkbook. Next, she developed Capgras syndrome, mistaking loved ones for impostors. The world her mother knew became suddenly foreign, says Loeb: “She'd say, ‘How did they get this apartment to look exactly like my other one? All the furniture is the same.'"
RELATED: Dementia's gender disparity: Report uncovers unique challenges facing women
In other patients, LBD can also cause motor issues, Loeb says, and frightening hallucinations. “The lamp in a room will look like a monster,” she says. “Caregivers make sure to put knives away.”

































































More on entertainment
A Moving Documentary About the Search for an Alzheimer's Cure
'Turning Point' shines light on drug researchers' determinationBruce Dern Explores the Theft of Genius by Alzheimer's Disease in 'The Artist's Wife'
In his new film, he takes on the complex challenge of portraying dementiaInterview With 'Moonlight Sonata' Director
Film is a study of deafness, dementia and hope