Staying Fit
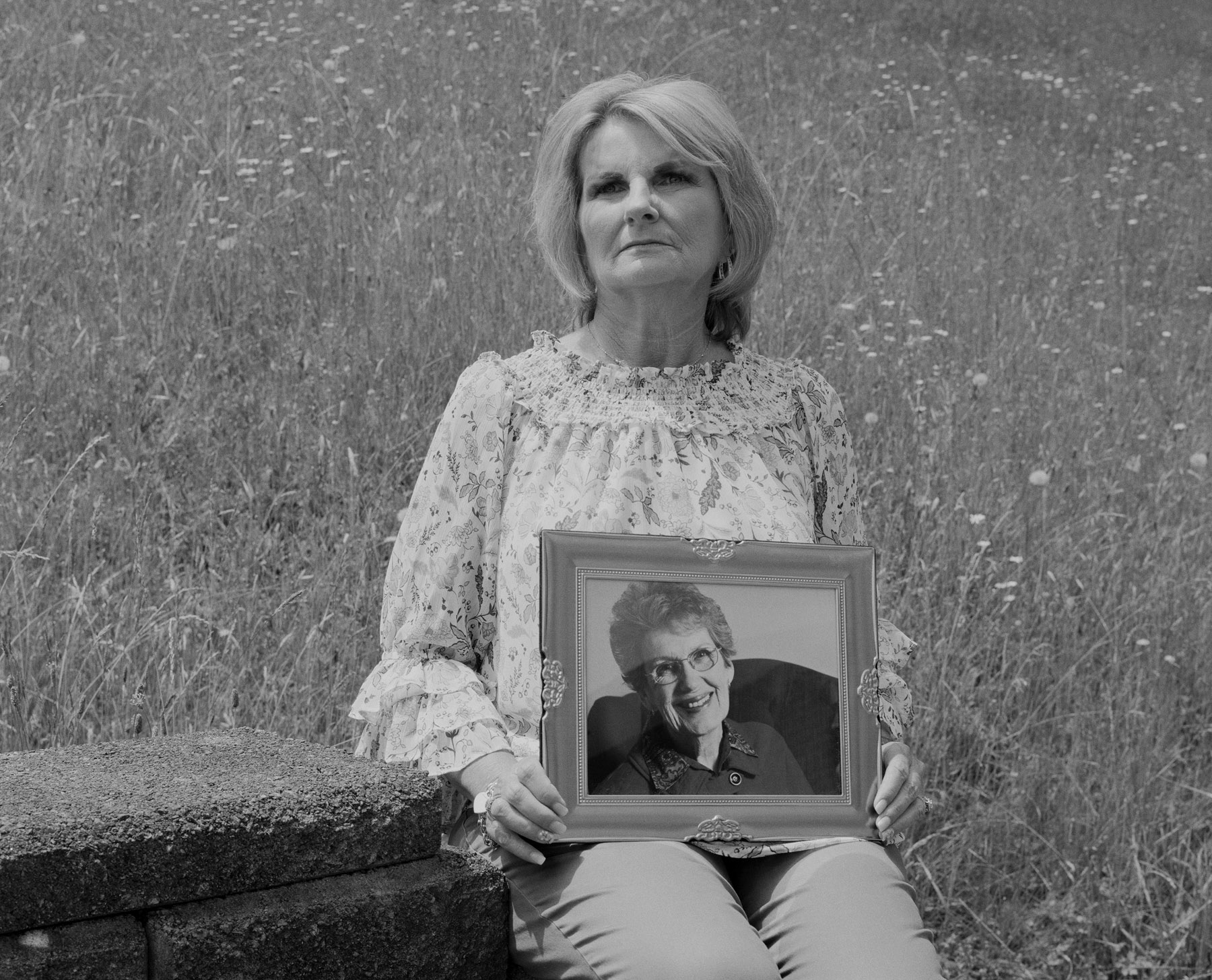
Betty Jo Artrip's favorite spot in Mountain View Regional Hospital, her nursing home of more than seven years, was the window at the end of her corridor. She affectionately called the spot the ridge,
for its view of an Appalachian mountain. It wasn't the most spectacular vista — more of a hillside than a hilltop — but she loved it, nonetheless.
Most days, after breakfast and a bath, Betty would roll down to the ridge in her wheelchair to meet her friend Amanda. Dementia hindered their ability to communicate much, but they enjoyed each other's company as they peered out from the fourth floor together.

The view from the ridge
In July 2022, Ballad Health — a large nonprofit health care chain serving mainly northeast Tennessee and southwest Virginia — announced it was closing Mountain View. The 44-bed nursing home in the small town of Norton, Virginia, was fueling “excess capacity” in the region, according to a letter from Ballad Health to its employees. In other words, too many nursing home beds were going unused. The 20 long-term care residents who lived there, including Betty, would have to find new homes.
The residents were formally given until April 2023 to relocate. But several staff and family members of residents claim they felt pressure from Mountain View's management to relocate residents as quickly as possible. By mid-September 2022, all the residents were out.
Betty struggled to adjust to her new 97-bed nursing home. She became confused, anxious and fearful, according to Jerry Artrip, Betty's youngest son. Then, “it was almost like a depression came over her,” Jerry recalls. After roughly five weeks in the new facility, Betty died. She was 93.
The deaths kept coming. Seven Mountain View residents died less than three months after their moves. Of the 18 residents who were relocated (two residents died before their transfers), only seven survive today. Though death rates among nursing home residents are typically high, Mountain View staff and families say the losses were excessive.
“If we had one or two [residents] pass away a year, that was a lot to us,” says Misty Mullins, who worked as a certified nursing assistant at Mountain View for almost a decade. “The move was killing people.”
Ballad Health declined AARP's requests for interviews.
Negative impacts from relocating fragile residents — often labeled transfer traumas — have long been a problem for U.S. nursing homes. For decades, resident advocates have warned of the harmful effects of involuntary moves and fought to increase protections against them. They say a chronic lack of oversight and accountability in the industry has allowed the problem to persist, often unnoticed.
That problem, with tragic consequences, may be about to grow. The COVID-19 pandemic threw the U.S. nursing home industry into turmoil, exposing an array of long-standing industry shortfalls from understaffing to overcrowding. The chaos pushed a growing number of facilities toward closure or consolidation, putting their residents at risk of displacement. Earlier this week, a St. Louis nursing home quickly shuttered its doors, making headlines as 170 residents were transferred elsewhere, some without their belongings or the knowledge of their families, The New York Times and other outlets reported.
Operating pressures and demands for improved performance have continued to mount. A proposed federal law designed to boost safety in these facilities by increasing staffing will likely add to the pressure. Roughly a quarter of nursing home residents nationwide may need to relocate once the rule takes effect, according to a recent analysis commissioned by the American Health Care Association (AHCA), the nation's largest lobbying group for nursing homes.
Without better uptake and enforcement of safeguards that allow for smooth transfers, many residents may be vulnerable to the trauma of upheaval, just like those at Mountain View.
After Relocation: A Surge in Deaths
20 Mountain View residents were told to find new homes in July 2022.
7 residents died less than 3 months after their transfers.
3 others died less than 6 months after theirs.
Of the 18 residents who were relocated (2 residents died before their transfers), only 7 survive today.
Residents were ‘dwindling away’
The term “transfer trauma” was first coined in the 1960s, when gerontologists started to worry that involuntary relocation of older people from private homes to institutions or between institutions could have an adverse effect on health and even cause death. In 1992, “relocation stress syndrome” (RSS) — a more clinical term for transfer trauma — became an official diagnosis of the North American Nursing Diagnosis Association (now NANDA International). Today, RSS is defined as “a state in which an individual experiences confusion and difficulty in adjusting to a new environment as a result of relocation.”
A small collection of studies involving nursing home residents shows that those who are involuntarily relocated may experience functional decline, increased loneliness and isolation, more hospitalizations and falls, and even death.
“Change is never easy,” says Debra Saliba, a geriatrician and professor of medicine at the University of California, Los Angeles. “Even bingo moving from one night to another can be hard.” Relocations are “huge adjustments,” she says.
That's particularly so for transfers involving dementia patients, who make up roughly 50 percent of all long-stay nursing home residents in the U.S. These patients commonly experience fear, disorientation and confusion at higher levels, says Kim Warchol, an occupational therapist and founder of Dementia Care Specialists, a company providing memory-care training.

Most of Mountain View's residents suffered from dementia, so nurses worked hard to keep routines consistent and familiar. Catering to the unique needs of each resident was key, says Caroline Haynes, a licensed practical nurse who worked on the long-term care ward.
The facility was opened in 1948 as St. Mary's Hospital by a group of nuns who'd emigrated from Ireland and England. Their mission was to serve “with dignity and a high degree of excellence, ever mindful of the privilege of taking care of the needs of the poor,” according to their founding statement.
Most of Mountain View's residents suffered from dementia, so nurses worked hard to keep routines consistent and familiar. Catering to the unique needs of each resident was key, says Caroline Haynes, a licensed practical nurse who worked on the long-term care ward.
The facility was opened in 1948 as St. Mary's Hospital by a group of nuns who'd emigrated from Ireland and England. Their mission was to serve “with dignity and a high degree of excellence, ever mindful of the privilege of taking care of the needs of the poor,” according to their founding statement.
“They treated their staff and patients as family,” says Haynes, who began visiting St. Mary's as a three-year-old in 1966 when her mother became the facility's director of medical records. When Haynes, now 60, was in her early 20s, she became a nursing assistant at what had by then become Mountain View. She left for a time but returned in 2015 and stayed on through the closure. “All of us that have worked there carried on the sisters' level of care,” she says.
Video: The Sisters' Legacy Caroline Haynes, former nurse of Mountain View, on the history of the nursing home and its closure.
That's what attracted Mullins, the certified nursing assistant, to Mountain View more than a decade ago. As the nursing home industry moved toward large, for-profit models with high patient-to-staff ratios, Mullins recognized that Mountain View's small size and intimate culture was rare. She was able to spend extra time with residents, letting them choose their clothes for the day and singing along as she played their favorite tunes. She made sure they always got a long soak: “I'd give 'em a bath like I would want to be bathed,” she says.
Amid the transfers at Mountain View, Mullins tried her best to uphold the sisters' legacy. She picked up shifts at the facility where most residents moved to try to help them adjust. There, she was required to care for about 12 residents per shift instead of eight. Still, she worked hard to provide her longtime patients with their normal standard of care. She even coordinated with other nurses to cluster them together on the same ward, so they would see familiar faces. When she worked the morning shift, she made sure they still got a good bath, even if it was shorter than usual.
‘She just started to look through me.’
But Mullins watched as the health of her Mountain View residents began to fail. Some stopped talking. A few stopped recognizing her and fell into what she called “a trance.” Many who used to travel the corridors of Mountain View in their wheelchairs for most of her 12-hour shifts would no longer leave their bedrooms. “They were just sitting in corners,” she says, “dwindling away.”
Lucille (Lucy) Trent was one of those residents. At Mountain View, where she lived for roughly four years, she did “exceptionally well,” says her youngest daughter, Kim Meade. Despite having dementia, Trent was almost always calm and content. The workers knew what she liked: being called “mommy,” sitting by the communal television, and bottles of Coca-Cola. “All she had to do was call out ‘Hello?’ and it didn't matter who was walking by, they would go and get her a Coke,” Meade says. “It was her thing.”
But after her transfer, getting Trent to eat or drink became increasingly difficult. After just a month in her new facility, her bottles of Coke remained full. “It got to a point where she wouldn't eat anything at all,” Meade says. “She just started to look through me.”
Trent died just shy of three months after her transfer at age 94. Chronic obstructive pulmonary disease was listed as Trent’s official cause of death. Meade says the move was at the heart of her decline.

Family photographs of former Mountain View resident Lucille Trent, who loved quilting and cooking. Kim Meade believes transfer trauma caused her mother's decline: “I really feel that's what happened to her.”
An industry on shaky ground
For decades, the nursing home industry has been shrinking: National occupancy rates and the number of facilities and residents have all steadily declined as aging adults increasingly opt for less institutionalized care. The declines persist even as the number of older Americans surges.
During the COVID-19 pandemic, about 580 nursing homes closed nationwide, according to a report by the AHCA. “A workforce crisis combined with chronic underfunding and soaring costs are currently the main reasons for closures,” the AHCA wrote in a statement to AARP. As a result, about 21,500 residents — or nearly 2 percent of the national nursing home population — have been displaced, the report found.
That number could surge, the industry claims. A first-of-its-kind federal law aiming to fix widespread understaffing in nursing homes with mandatory minimum staffing levels is expected to take effect in 2024. A recent analysis of the new law by the advisory firm CliftonLarsonAllen, commissioned by the AHCA, projects nearly 290,000 residents — almost a quarter of nursing home residents nationwide — could be at risk of displacement under it.
With complex medical cases, things can easily fall through the cracks.
Nursing home operators claim they can't find enough workers and can't afford extra staffing to meet the mandate, which CliftonLarsonAllen estimates will be $6.8 billion nationally. The industry has lost roughly 150,000 workers, or about 10 percent of its workforce, since the onset of the pandemic. Low pay, dangerous working conditions and high rates of burnout from understaffing have led to this mass exodus, nursing home critics argue.
Although there's risk of transfer trauma for displaced nursing home residents, their advocates argue there's also risk in keeping them in facilities without the workforce to support their needs. “Inadequate staffing can have dangerous — even deadly — consequences,” says Megan O'Reilly, AARP vice president for health and family issues. AARP supports the introduction of staffing minimums. “This is one critical way to ensure quality of care,” O'Reilly says.
If some nursing homes fold under the mounting regulatory pressures, maybe that's “for the best,” argues Charlene Harrington, a professor emeritus at the University of California, San Francisco (UCSF), who has documented widespread care deficiencies in her research on nursing homes. “Nursing homes are, generally, not of sufficient quality ... and there are a lot of people in nursing homes that don't need to be in there.” Continued industry contraction, in tandem with more long-term care alternatives, including home health services, will benefit America's aging population, she says.
But nursing homes will still be needed. So exactly which nursing homes close and in which communities is important, Harrington says. Large, for-profit chain facilities are more likely to stay in business, she says, while smaller, nonprofit operations, which tend to provide better care, go under. In rural areas, such as Norton, Virginia, where Mountain View was located, quality care alternatives are limited, so these closures are particularly worrying.
When shutdowns are necessary, some strategies can reduce the risks of transfer trauma, resident advocates say. Relocation is “not ideal” among this fragile population, says Elizabeth Halifax, an assistant professor of social behavioral sciences and nursing home researcher at UCSF, “but you can make it as painless as possible.”
Safeguards are written into federal nursing home regulations, including notifications at least 60 days before closing, state approval of a facility's closure plan and assurances that residents are “transferred to the most appropriate facility or other setting” that considers their needs and best interests. Essential care documents and information must be given to the receiving health care provider.
But amid complex medical cases and needs, things can easily fall through the cracks, says Joseph G. Ouslander, a professor of geriatric medicine at Florida Atlantic University. No shared system of electronic health records exists for nursing homes, making the transfer process ripe for medical errors. “They happen all the time,” he says.
For dementia patient Georgia Durham, the tipping point of her transfer may have been the loss of her hearing aids, which disappeared in the flurry of activity before her move out of Mountain View, says her youngest son, Jerry. “She really relied on those,” he says.
Without hearing aids, Georgia struggled to acclimate to her new home. Unable to listen to the Christian music she loved, her regular programs on Fox News or the familiar voices of her sons, she became less engaged and seemed depressed, Jerry says. Ten weeks after her relocation, Georgia, 88, contracted COVID-19 and died less than 24 hours after testing positive for the virus. Amid the move, she'd “maybe lost her will to live,” Jerry says.


Georgia Durham loved dressing up and playing with her great-grandchildren. Her youngest son, Jerry, says he'd “give anything” to have more time with his mother.
Failing safeguards
Though the list of regulations to safeguard against transfer trauma is long, proper adoption of them has historically been weak, says Lori Smetanka, executive director of the National Consumer Voice for Quality Long-Term Care. Complaints regarding improper discharge or transfer have consistently been among the most common types of grievances reported to the States' Long-Term Care Ombudsman Programs for roughly a decade.
At the same time, the government doesn't collect national-level data on resident transfers or discharges occurring in nursing homes. The Centers for Medicare & Medicaid Services (CMS), the government agency responsible for regulating the vast majority of U.S. nursing homes, says it provides oversight through surveys and other means to make sure institutions comply with federal requirements, according to a CMS spokesperson. But CMS data shows that roughly 30 percent of the nation's nursing homes are overdue on these surveys, which by law should occur at least once every 15 months.
Even when facilities are inspected for their transfer processes, there are few penalties for violating safeguards, so there's little incentive for nursing homes to comply, says Toby Edelman, a senior policy attorney for the Center for Medicare Advocacy, a legal nonprofit working to advance access to health care coverage.
A high-profile example of these failing safeguards is the turmoil that unfolded at San Francisco's Laguna Honda Hospital and Rehabilitation Center, a skilled nursing facility serving about 700 low-income patients. In April 2022, the federal government stripped the then-156-year-old facility of its Medicaid certification, and therefore its government funding, due to substandard care. Administrators were told they had until mid-September to get everyone out.
At least 11 of the first 57 residents transferred out of Laguna Honda died shortly after relocating. A state investigation noted that Laguna Honda missed critical steps to minimize possible transfer traumas, failing to properly assess residents' conditions, develop and implement individualized care plans, and report residents' care needs to their receiving facilities' physicians. The facility was fined $36,000 for the offenses.
‘In the end, it's all about money, not care and love.’
In a statement to AARP, Laguna Honda officials disagreed with the state's findings and blamed federal regulators for issuing an “entirely insufficient” four-month deadline to transfer nearly 700 medically fragile residents.
Both were culpable, argues Patricia McGinnis, executive director of California Advocates for Nursing Home Reform. Government regulators played a lead role in endangering the residents
by pressuring Laguna Honda to evict residents quickly, knowing it had no safe places to send them,
she wrote in a January public statement. The fines handed down to the facility were a mere slap on the wrist for repeated and lethal acts of elder abuse.
Under an intense media spotlight, the federal government extended Laguna Honda's funding to allow for better closure planning and an opportunity to win back its Medicaid certification. In August 2023, recertification was granted, meaning the facility could keep operating.


Before her death, Betty Artrip enjoyed spending time with her sons and the Mountain View nurses. Jerry, Betty's youngest son, sits with his wife, Rebecca, at his mother's gravesite.
Left in the dark
No such spotlight ever came to Mountain View. Instead, workers and family members of residents say they were left to deal with the fallout of the closure of their small rural facility on their own.
Virginia's Long-Term Care Ombudsman Program became aware of Mountain View's closure when it was publicly announced and offered support. But Mountain View officials declined help from the ombudsman program and “indicated that full assistance was being provided to residents and their families,” Joani Latimer, who heads the program, wrote to AARP. No official complaints about the facility were received, she added, which is typically required for the program to intervene.
Several Mountain View staff and family members say they would have welcomed support. After news of the closure, they spent hours researching and comparing care alternatives, touring new facilities, filling out paperwork, packing and unpacking and, eventually, trying to nurse residents back to health after their transfers.
Many felt pressure to act swiftly, worried loved one would miss out on a bed at the next-best or next-closest facility if they waited. Others feared a COVID-19 surge in the region could suddenly halt admissions at facilities, leaving their loved ones with no place to go. Meade believes the rush was harmful. “I wish they hadn't taken her so fast,” she says of her mother. “I think that was a mistake.”
Video: “The Closure,” poem written and read by Jerry Artrip Jerry Artrip's mother, Betty, died five weeks after being transferred out of Mountain View.
Jerry Artrip has struggled to process his feelings about the experience, even turning to poetry to try to find the right words. Since his mother's death, he's spent months searching for explanations for Mountain View's closure, but responses from Ballad have been brief. “They've said it's just a business decision,” he says. “In the end, it's all about money, not care and love.”
Jerry Durham admits more time probably wouldn't have changed the outcome. “I think the move was always going to be too much for her,” he says of his mother. But he believes a pause on transfers would have at least allowed him a few extra months with her. “I would give anything for that.”
Emily Paulin is an editor at aarp.org who covers nursing homes, health care, and federal and state policy. Her work has also appeared in Broadsheet, an Australian lifestyle publication.