FEATURe STORY
A Fighting Chance
His father, a devoted football fan, was diagnosed with an aggressive cancer. So writer Jamie Metzl went on offense, exploring every emerging treatment. Here, he shares what he learned about finding the most promising care for someone you love

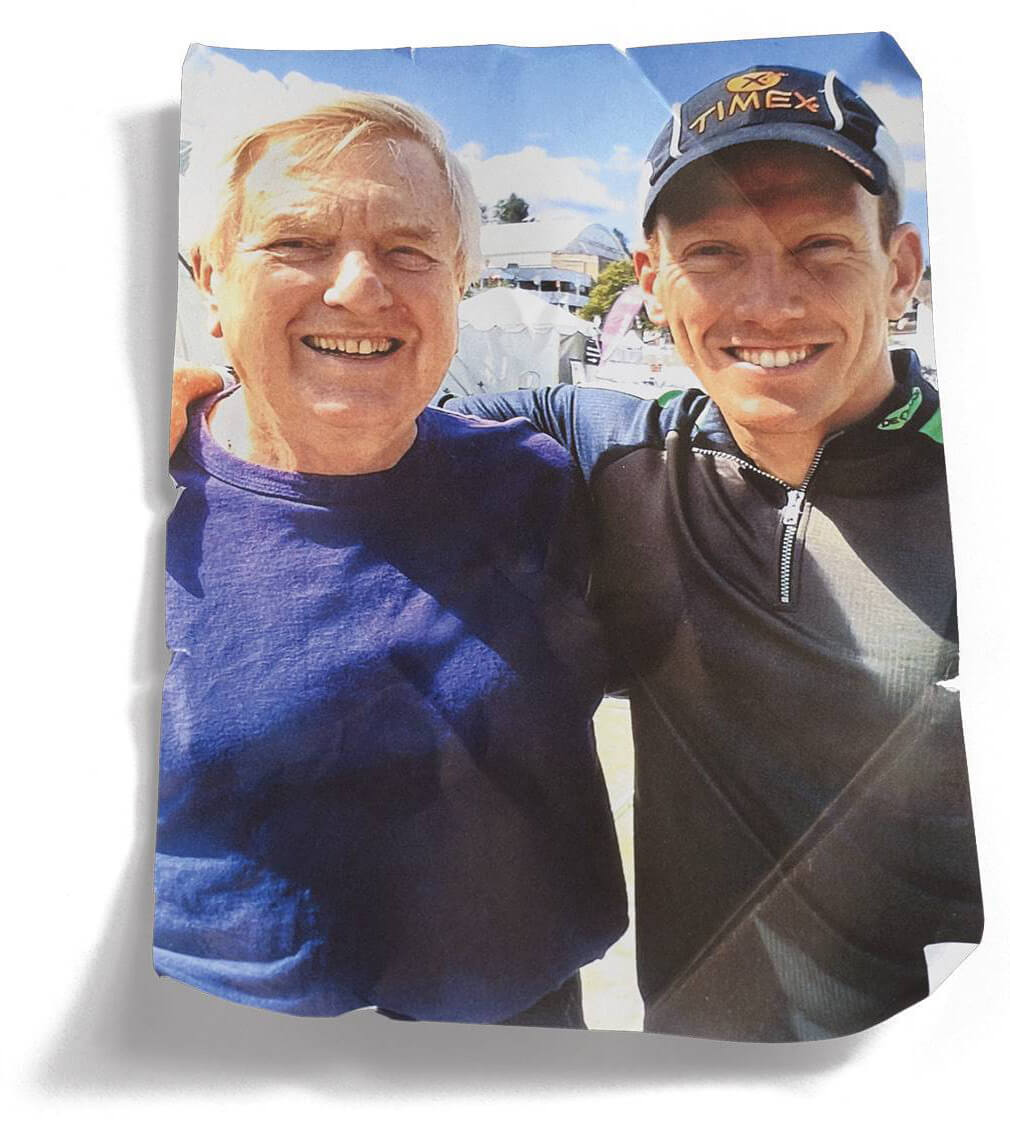
Jamie, left, dad Kurt and brother Jordan at the 2024 Super Bowl
“YOU HAVE CANCER.”
There are perhaps no three words more frightening than these. Yet nearly 4 in 10 of us will hear them at some point in our lives. When we include relatives and close friends in that mix, the experience of a cancer diagnosis is near universal.
And the next words, inevitably, are: What now?
In April 2025, my beloved father, Kurt Metzl, passed away two weeks shy of his 90th birthday after a heroic, nearly three-year battle with stage 4 metastatic neuroendocrine cancer—a rare and deadly cancer of the cells that receive signals from the nervous system and release hormones into the bloodstream.
It was the most painful moment of my life to date. But I was also grateful for the fact that he had survived far longer after his diagnosis than his doctors, and the medical literature, had predicted.
Although we’d been told he had no more than a year of healthy life left, we beat those odds as a result of a remarkable team effort. In those extra years of life, my father celebrated the bat mitzvah of his oldest granddaughter, multiple holidays and two stunning, come-from-behind Super Bowl victories by his cherished Kansas City Chiefs.
But this story is not just about my father. It’s about how all people diagnosed with cancer, and their families, can play a crucial role in contributing to the quality of their care and increasing the odds of the best possible outcomes. It’s about how, after the horrifying mix of fear, sadness, confusion and even helplessness that accompanies any cancer diagnosis, patients and their families can harness a force that can sometimes be even more impactful than fast-reproducing cancer cells: informed and empowered hope.
Two weeks before his death, I read my dad an early draft of this article, about how other cancer patients and their families might use the lessons we’d learned to extend and enrich their own lives. With tears in his eyes, he told me he’d do anything to help others facing his same long odds after a cancer diagnosis.
This is what he wanted you to know.
Suiting Up for the Fight
At the time of my father’s initial diagnosis in September 2022, his scans showed that the cancer was growing quickly: His widely circulating, hormone-releasing cancer cells were primed to spread to multiple organs. More tests still needed to be done, we were told, but probably the best we could hope for would be to temporarily slow the cancer’s spread before things got much worse, likely within a year.
I was in shock. I’d always thought my father was indestructible. He was, after all, a survivor.
He and his parents had escaped Nazi Austria in 1938 and then spent a decade as displaced persons in Switzerland before finally emigrating to the United States in 1948, when my dad was 13. They settled in Kansas City, Missouri, where my father quickly learned English, became a star student and began his lifelong passion for Kansas City sports teams.
Advances in technology have been slow to reach many patients.
After completing medical school just across state lines at the University of Kansas, my father headed to New York City for his pediatrics residency. There he met and wooed a brilliant blond speech pathologist—my future mother, Marilyn—and brought her back to the Paris of the Plains, where my three brothers and I were raised. My dad became a pediatrician, serving the community for more than five decades, and my mother a psychologist. They were community leaders, avid bikers, fearless skiers and, of course, Chiefs season-ticket holders.
After 57 years in Kansas City and more than a year before my father’s cancer diagnosis, my parents moved to Denver to be closer to my younger brother’s family. That’s where my two other brothers and I rushed when we got the news. Soon after we arrived, my father wept over the prospect of missing his oldest granddaughter’s bat mitzvah the following year. He told me emphatically that he wanted to fight for as much time as possible.
Handing him the red-and-gold Chiefs beanie I’d brought for him, I told him that just like Patrick Mahomes rallying his team in the face of impossible odds, we were going to fight for every minute of possible time.
He put on his new uniform with determination.
How to Get the Care You Deserve
I am a technology and health care futurist who writes books and speaks to hospital boards and medical associations about the future of health care. Based on my work, I knew well that with the remarkable progress in oncology, a cancer diagnosis now means something different than it did just a few years ago. Incredible advances in modern medicine have reduced the overall death rate from cancer in the U.S. by more than a third over the past three decades and led to significant increases in the average amount of time people live after initial cancer diagnoses.
But improvement in cancer care is only one part of the story. While there’s been astounding progress in medical research, clinical trials and cutting-edge applications, even the most beneficial new treatments are often unevenly distributed among medical centers and slow to reach patients. The faster our technology advances, the harder it is for all of us to keep up, including health care providers. This creates an essential need for patients and their families to step up in new ways. Although it may at first seem daunting, and requires a bit of work, the opportunity to gather information and help shape our own care, and that of the people we love, is available to every one of us.
I wanted my father to be treated as if the exciting future of medicine had already arrived. To make that happen, I knew that we needed to play an active role.
After hearing the preliminary diagnosis of cancer from my father’s internist, our first step was to learn as much as possible, quickly and accurately, about the particular cancer that we were going to fight. An interventional radiologist performed a biopsy that showed my father had a type of neuroendocrine cancer.
Dad Kurt with Jamie at the Lake Placid Ironman, 2007
Even with my knowledge of cancer in general, as well as our family’s medical background (in addition to my dad, my three brothers are also M.D.s), we knew next to nothing about neuroendocrine cancer at the time of my father’s diagnosis. To bridge that gap, I began poring over the many online materials specifically tailored to his cancer, including the website of the Neuroendocrine Tumor Research Foundation, and listening to its superb podcast, NETwise, on my daily runs. These types of resources are available, free of charge, to everyone, for a remarkably broad range of cancer types. (Start with one of the resources listed in step 1 of “Your 15-Point Cancer Battle Plan,” below.)
Recognizing that I needed more help, I reached out to Cancer Commons (cancercommons.org), a resource that brings together critical links and information about a wide range of cancers. Other outstanding resources include the highly informative American Cancer Society, CancerCare, Cancer Support Community and OncoLink websites. (I cannot overemphasize the importance of learning everything you can about the exact type of cancer that’s threatening you or a loved one, as quickly as possible. The resources are free.)
Cancer Commons also designates, for free, specialists to advise patients and their families remotely. Ours was a caring and knowledgeable woman who had served for decades as an oncology nurse. Like a great football coach, she quickly proved invaluable by helping me better understand the essential steps we needed to consider right away, before we even had an oncologist assigned.
Analyze the Enemy
The first thing I suggested to my father’s internist in the earliest days following his diagnosis was that we consider whole genome sequencing (WGS) my dad’s cancer cells at the earliest possible moment. This standard of care, when ordered by a doctor, may be covered by Medicare after a stage 3 or stage 4 diagnosis and ideally should be one of the very first steps after all late-stage cancer diagnoses. (Unfortunately, only a small percentage of cancer patients, including those with late-stage cancers, asks about this sequencing, which can play a critical role in developing a treatment protocol.)
The internist had not planned on ordering this test immediately, because doing so was not the normal standard of care for my dad’s type of cancer, at least not this early in the medical process. But we knew from the early tests that the cancer was spreading rapidly and that gathering potentially actionable information as early as possible could help our crucial, early-stage decision-making.
A relatively new form of precision medicine, WGS involves extracting and sequencing DNA from a tumor and comparing it with the DNA from the patient’s noncancerous cells. Understanding these differences helps doctors look for essential genetic mutations that impact how cancer cells spread. When there’s a match between the mutation and an available treatment, these mutations can potentially be targeted precisely.
After the internist agreed to order the WGS, I asked her to consider prescribing another, more experimental diagnostic tool she had never used before: a patient-derived tumor organoid test. The process involves extracting tumor cells from a patient, growing these cells in a lab and then dividing them into tens or hundreds of batches—essentially, growing miniature versions of the tumor, clusters of cells that are known as cancer organoids. This allows for multiple drugs and drug combinations to be tested on identical twins of the patient’s cancer cells in a lab setting. If a certain treatment kills or shrinks the clusters of cancer cells better than others in the lab, there’s a decent chance that treatment may be more effective inside the person.
As with the genome sequencing, the sooner we extracted the cancer cells and sent them in, the sooner we’d have information that could prove important to my dad’s care. His pathologist overnighted the collected biopsies to an organoid laboratory in Seattle.
All this happened very quickly in those critical first weeks after my father’s initial diagnosis. When we finally had a specialized oncologist assigned to us, I wasn’t sure how that person would feel about my having been so involved in my father's care. I secretly feared he might consider me less a member of the team and more like one of those crazy fans streaking across the football field being chased by security guards.
Build a Great Team
It’s probably a function of human aging that the older we get, the younger young people start to look. So as a guy in his 50s, I was taken aback when our new oncologist first walked into the examination room. My initial twinge of concern about his youth was completely off the mark: He knew far more about cancer than I ever would, and his wisdom and open-mindedness were the greatest assets we could have hoped for. We quickly began working as a team.
Our oncologist suggested we start treatment with a relatively standard and generally well-tolerated oral chemotherapy. With his blessing, I also sought a second opinion from physicians at Harvard, who concurred.
Never taking off his Chiefs hat during waking hours, even long after the season had ended, my dad religiously took his daily chemotherapy pills. He tolerated the treatment well; attended, with my mom, nearly all of his granddaughters’ soccer games; and was proud to keep all of his once famously red hair. His mood was massively boosted when the Chiefs clinched a shocking Super Bowl victory against the highly favored Philadelphia Eagles in February 2023.
Sequencing the genes from my dad’s cancer cells allowed us to identify potentially effective treatments more quickly.
But when we got the results back from his post-chemo scans a few weeks after the game, we were disheartened to learn that the cancer was still growing. Our oncologist recommended as a next step a well-studied and much more aggressive form of intravenous chemotherapy that had about a 30 percent chance of helping but was virtually certain to cause major side effects and knock my father on his rear. I worried that, at his age, he might never get back up and felt desperate to help find a better alternative. It’s a common, and difficult, choice that many families face.
That’s when we learned just how crucial our sequencing of those early cancer cells had been. The sequence report showed that a specific mutation in my dad’s cancer cells—one that was extremely rare in my dad’s form of cancer but less rare in some others—was operating as a drill sergeant, instructing those cells to keep growing. Fortunately, a drug already existed for blocking the expression of this mutation. It had been used to treat other cancers but had hardly been used to treat my dad’s type of cancer.
It was a risk. The medical literature indicated that this drug had been used to treat just 29 patients with multiple tumor types containing the same specific mutation as my father’s—including four people with neuroendocrine cancer—and had helped more than a third of those patients. But those odds were similar to what the harsher and more traditional treatment offered. The best we were told to hope for with this new therapy might be a slowing of the cancer’s spread—not a remission—but it was likely that my dad would tolerate it better than the chemo. I felt that the potential benefit of this approach outweighed the potential risks, at least in comparison to our alternative. Together, the oncologist and our family weighed the pros and cons of the two different approaches and decided to forgo the rough chemotherapy that the oncologist had initially recommended for this more targeted method.
Celebrate the Wins
My dad needed to take the new pills twice a day for a couple of months before we’d be able to test whether they were working. As the date of the new tests approached, I felt extremely nervous. Had the experimental therapy kept my dad’s tumor from growing?
As our oncologist walked us through the new images on his computer, it felt like Patrick Mahomes and the Chiefs pulling off another come-from-behind miracle. Not only had the treatment arrested tumor growth, but the new scans showed remarkable remission in all of my dad’s organs. We could see the groupings of cancer cells withering as the normal cells and my dad’s immune system fought back.

Kurt in his pediatrics office, adorned in Chiefs memorabilia and a stethoscope, in the photo used for his obituary
As a result of this progress, not only did he attend the bat mitzvah later that year, but he and my mother together recited a special prayer for their granddaughter at the altar, then danced with our entire family at the party that night.
In February 2024 my brother Jordan and I decided to celebrate our father’s amazing progress by flying him to Las Vegas for his first in-person Super Bowl: the Chiefs against the San Francisco 49ers. Jordan collaborates with ESPN on occasion; when he informed them that our Holocaust- and cancer-surviving Chiefs superfan dad was coming to the game, they pulled out all the stops. Entering the penthouse hotel suite they had secured for him, he stopped in his tracks. His bed was covered in Chiefs swag, including a helmet signed by Mahomes himself.
After all that anticipation, we sat nervously in our seats the next day as the 49ers outplayed the Chiefs, who seemed to be collapsing under the pressure. But my father, proudly sporting his Chiefs hat, refused to give up hope. And just when the game seemed all but lost, Mahomes somehow rallied the team to a last-minute field goal to put the game into heart-thumping overtime. When he later spiraled a perfect pass to Mecole Hardman in the end zone to clinch the win, our two stories of beating impossible odds came together for one glorious moment.
The End of a Miraculous Season
But even perfect moments cannot last forever. After two years of remarkable remission, my dad’s cancer started growing back aggressively in late 2024. We tried new approaches to fight back. Some worked better than others, but the cancer marched on. Searching for more miracles, we fought, yard by yard, day by day, minute by minute, for more health and more time while we cherished the health and time we had.
By early 2025, soon after Mahomes and the Chiefs fell to the Philadelphia Eagles in Super Bowl LIX, our family huddled around my father as his condition markedly waned. The weekend before my dad died, we gathered in Denver to celebrate his 90th birthday three weeks early and hold a Passover seder commemorating everything he, our family and all people seeking a better future had achieved in our continual struggle for freedom, opportunity and hope. Less than a week later, he was gone.
My father fought, and lived, and loved life to the very end. The photograph we chose for his obituary showed him at his pediatrics office wearing a Chiefs apron and hat with a stethoscope around his neck and the huge smile that had been the hallmark of his life and medical career.
In addition to his personal and professional legacy, my father left us one more gift: The targeted treatment approach we had pioneered with our oncologist had shown such dramatic results that he published a case report in the Journal of Gastrointestinal Cancer recommending that it be considered a new, potential first-line approach for others with my dad’s particular cancer. Dad’s hope would come true: The legacy of our struggle against his cancer would help others in theirs.
Jamie Metzl is a technology and health care futurist and a commissioner of the Lancet Commission on Precision Medicine. He is the author of six books, including Superconvergence: How the Genetics, Biotech, and AI Revolutions Will Transform Our Lives, Work, and World.
Your 15-Point Cancer Battle Plan
There is only one way to respond to a cancer diagnosis: aggressively and creatively. Some of the most important decisions will be made early on, when patients and their families know the least and feel the most destabilized. Here are 15 important steps I recommend patients and their families take to help optimize their care:

1. Learn a lot, fast. Most cancer types have nonprofit associations, patient and family groups, and websites.
> Cancercommons.org (877-971-1200) provides free expert advisers to help patients explore their diagnoses and options.
> The Patient Advocate Foundation (patientadvocate.org, 800-532-5274) offers case management services and financial aid to Americans with chronic, life-threatening and debilitating illnesses.
> CancerCare.org (800-813-4673) furnishes free counseling, workshops and financial assistance.
Many hospitals and insurance programs provide similar services. In addition, most diseases, even rare cancers, have nonprofit organizations that can help you in your fight. (Try typing your diagnosis and “foundation” into your search bar.)
2. Find a great oncologist, and don’t be afraid of younger doctors. Although experience is extremely valuable, younger oncologists might be more up to date on the latest science. If you have a younger physician, ask them whether they are consulting with colleagues of other backgrounds.
3. Tell your oncologist right away that you’re hoping to be as informed and constructive as possible. Building trust with and within your care team is essential. Ask your oncologist what steps you can take to make your partnership as successful as possible.

4. Ask your doctor right away about having the cancer cells sequenced and grown as cancer organoids. These processes can often be initiated right away, sometimes even before you have a full diagnosis. While sequencing is becoming more commonplace, growing cancer organoids is considered more experimental.
5. Seek second opinions. Don’t be afraid to tell your care team that you are seeking an additional consultation. At its best, oncology is a team sport.
6. Think deeply about your priorities. Some patients might prioritize quality of life over aggressive treatments; others may choose survival at any cost. Doctors might think about the risks and rewards of various approaches differently than patients and their families.
7. Keep an ongoing list of questions. This is a stressful time, so feeling overwhelmed is natural. Keep jotting down any thoughts that occur to you or questions that arise.

8. Have loving and honest conversations with your family about end-of-life care and make sure you have an up-to-date living will describing your treatment and other preferences. You can download your state’s form on the AARP website: aarp.org/caregiving/financial-legal/free-printable-advance-directives. Once you fill out the form, you will need to have the document notarized or signed by two witnesses, depending on your state, before sharing it with your care team.
9. Respect the critical expertise of your care team but don’t take yourself out of the equation. Cancer care can be as much of an art as a science. The four most important steps are (1) finding the right and best possible care team, (2) getting the most appropriate diagnostic tests as quickly as possible, (3) determining the range of possible treatments and (4) deciding the order in which the applicable treatments will be administered. Educated patients and families can and should play a constructive role in all these decisions.
10. Learn about ongoing trials that may be relevant for your type of cancer on the U.S. government’s clinicaltrials.gov website.
11. Ask your care team about consulting with a nutritionist and a social worker, and make a plan for maintaining the healthiest possible diet and remaining active. Healthy eating and moving as much as possible can contribute significantly to your well-being. Even breathing exercises, yoga and daily walks can be extremely helpful, both physically and emotionally.

12. Invest in the support communities around you. Cancer can be terrifying and even isolating, but try your best not to feel alone. Connect with communities of patients and families who have received the same diagnosis; you can find support groups for various cancer types through the websites of the American Cancer Society and other cancer organizations.
13. Set up a home health-monitoring system. There are options for all budgets. They include wearing a device such as an Apple Watch or Oura Ring to monitor your heart rate, temperature, sleep and other vital signs, and checking your oxygen saturation each morning with a simple oximeter. Log these daily figures on your phone or in a notebook. If you see big changes, let your care team know.
14. Don’t be intimidated by statistics. Cancer survival rates are averages. They may not give you an accurate picture of your own chances for cure or remission. Hope is your greatest ally, so don’t give it up.
15. Embrace your life. Set big and exciting goals for family celebrations or other milestones. Your battle is about gaining time, happiness and meaning. Even after a cancer diagnosis, you’re just as alive as anyone else. New and wonderful memories are waiting to be made. Make them. —J.M.
The Future of Cancer Care
If a treatment works for enough people, it’s usually approved for everyone. That’s “generalized medicine”—medicine based on population averages.
But there’s a better way to treat malignant tumors: precision medicine, using treatments based on our own individual genomes. The future of precision medicine is coming faster in the field of oncology than most anywhere else. Here are some key developments:
Genome sequencing. Rather than identifying a cancer based on the tissue where it originated, this approach focuses on the unique molecular identities of a patient’s cancer cells. A cancer originating in a person’s lungs, for example, might be less like other people’s lung cancers in important ways and might respond better to an approach more often used to treat another type of cancer.
CAR T-cell therapy. In this approach, T cells—a type of white blood cell—are isolated from blood drawn from a patient with cancer. The scientists can then genetically manipulate these isolated T cells to optimize their innate cancer-fighting abilities before reinfusing them back into the patient.

Personalized cancer vaccines. Cancer vaccines instruct a patient’s body to protect itself against cancer cells. A number of different approaches, including mRNA-, DNA- and microbe-based vaccines, can stimulate the body to create an immune response against the cancer. —J.M.
Jeff Elkins (Courtesy Jamie Metzl); Jeff Elkins (Courtesy Jamie Metzl); Illustrations by Elias Stein; Jeff Elkins (Courtesy Jamie Metzl)