Your Health
IS PLATELET-RICH PLASMA THERAPY RIGHT FOR YOU?
Despite controversy and mixed results, PRP is racking up successes as a treatment for a variety of conditions
BY JEANNE DORIN MCDOWELL
The first thing John* smelled was his wife’s hair. Then coffee, sautéed scallops and compost—the first scents he’d experienced in 45 years.
In his 20s, John suffered a traumatic head injury that stole his sense of smell. At 73, he attempted one last-ditch medical intervention: platelet-rich plasma therapy, or PRP.
While PRP has been around since the 1970s, it took off in the 2000s, when sports medicine doctors began using it to help athletes recover from injuries. But in recent years, PRP has come out of the locker room; today it’s used to treat a wide variety of conditions: osteoarthritis, hair loss, vocal cord scarring, erectile dysfunction, vaginal atrophy, infertility, dry eyes and skin rejuvenation.
For John, PRP helped when nothing else could, says Dr. Zara Patel, director of the Stanford Initiative to Cure Smell and Taste Loss, who treated John in her clinic.
How PRP works
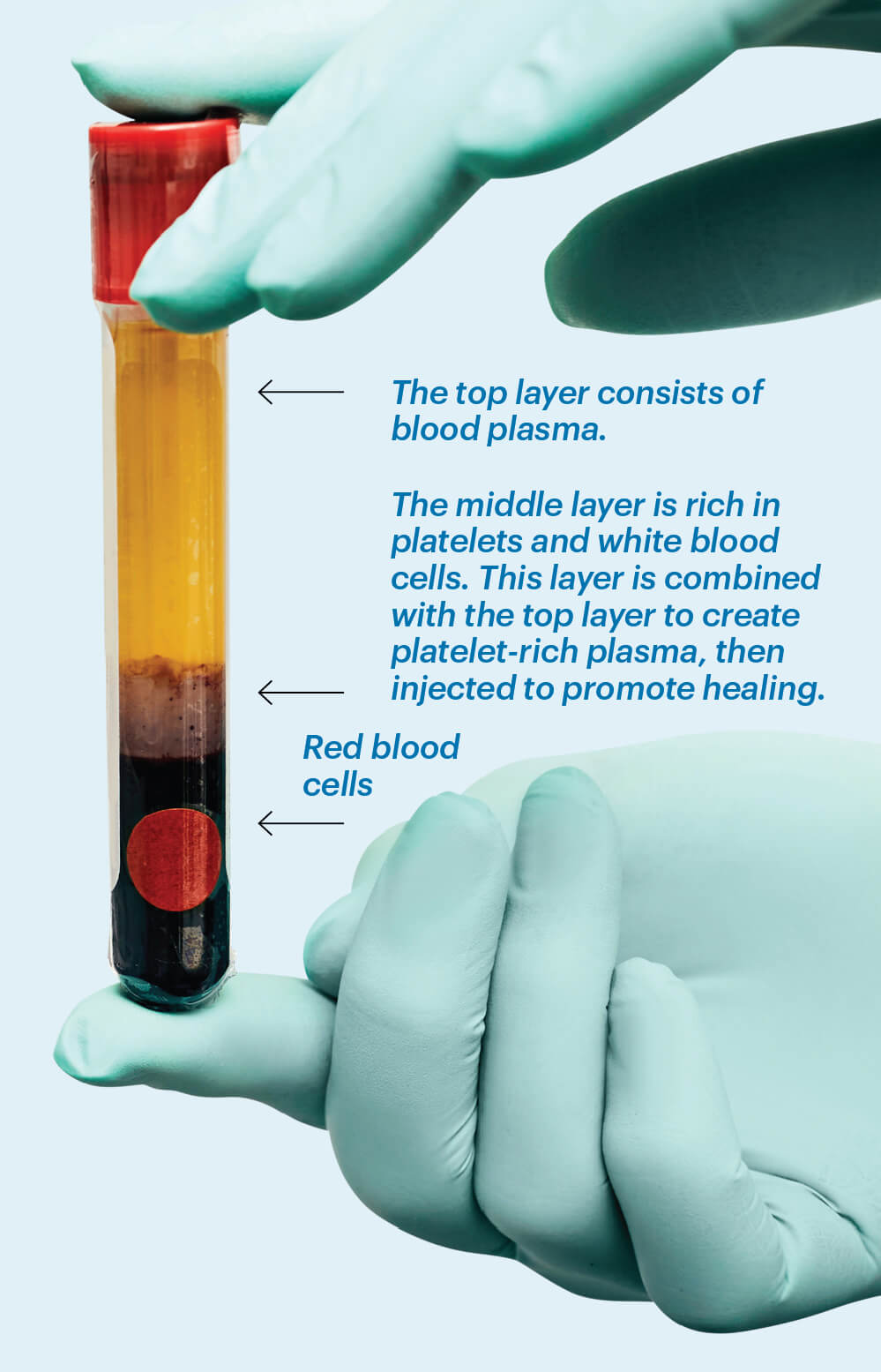
PRP uses the body’s own healing abilities to relieve pain and repair damaged tissue. A lab tech or doctor draws the patient’s blood and places it in a centrifuge, where it is spun to separate the blood into three layers: a bottom layer of dense red blood cells, a middle layer containing platelets and white blood cells, and a top layer of plasma. The middle layer is selected to create a concentrated volume of platelets that’s rich in growth factors, which can stimulate pain relief and improved function. This concentration is then combined with the plasma layer and injected into the injured area. Treatment sessions usually last about one hour, and several treatment sessions are often required.
Promising but uncertain
PRP is not fully accepted by the medical establishment—or reimbursed by insurance companies. Both the Osteoarthritis Research Society International and the American College of Rheumatology recommend against using PRP for osteoarthritis of the hip and knee, and the American Academy of Orthopaedic Surgeons supports PRP use on only a “limited” basis.
In part, reluctance to give PRP a full-throated endorsement is due to the inconsistency of study results. A randomized clinical trial published in JAMA in 2021 found that PRP injections did not significantly improve knee osteoarthritis symptoms after 12 months. But in 2025, a study published in The American Journal of Sports Medicine determined that PRP injections to the knee provided clinically significant pain relief, though it also called out the lack of standardization in PRP protocols. Variations in preparation methods, metrics, data collection and equipment could account for some of the inconsistency.
Because PRP is made from the body’s own blood, its quality is variable, says Dr. Bert Mandelbaum, an orthopedic sports surgeon and codirector of the Regenerative Orthobiologics Center at Cedars-Sinai in Los Angeles. Platelet density can fluctuate from day to day, depending on hormones, exercise and foods eaten, among other factors.
“When I prepare my patients, I tell them their own blood is their medicine, so they need to boost it as best they can,” says Dr. Alice Chen, a physiatrist with the Hospital for Special Surgery in Stamford, Connecticut. “I recommend they avoid alcohol and smoking for at least two weeks beforehand and reduce or eliminate sugar.”
Still, results are hard to predict. “Some people improve dramatically, and some don’t,” says Patel. And the procedure can be expensive as well: A number of factors can affect cost, but a single procedure is roughly $500 to $2,500, with patients often returning for more treatments.
“It’s important for the physician and patient to have a realistic discussion on what the outcome may be,” says Dr. Brennan Boettcher, a sports medicine physician at the Mayo Clinic in Rochester, Minnesota. “Some people don’t like paying out of pocket for something that may not help them.”
Regardless, it’s important that the doctor administering PRP therapy has your complete medical history, as those who have blood disorders, active cancers or autoimmune disorders may not be good candidates.
Even if you’re a perfect candidate for PRP, the potential results are hard to quantify, says Boettcher. “While we have many high-quality trials demonstrating efficacy, we need more comparative trials that look at what dose of PRP is correct, and more trials identifying factors that can lead to someone not seeing a benefit.”
*John is a pseudonym used to protect doctor- patient confidentiality.
Jeanne Dorin McDowell writes about health and wellness for national publications and websites.
PEAKSTOCK/SCIENCE SOURCE