Your Health
IS IT BRONCHITIS—OR PNEUMONIA?
These two diseases can look and feel the same, but they pose different risks. Here’s what to know
BY RACHEL NANIA
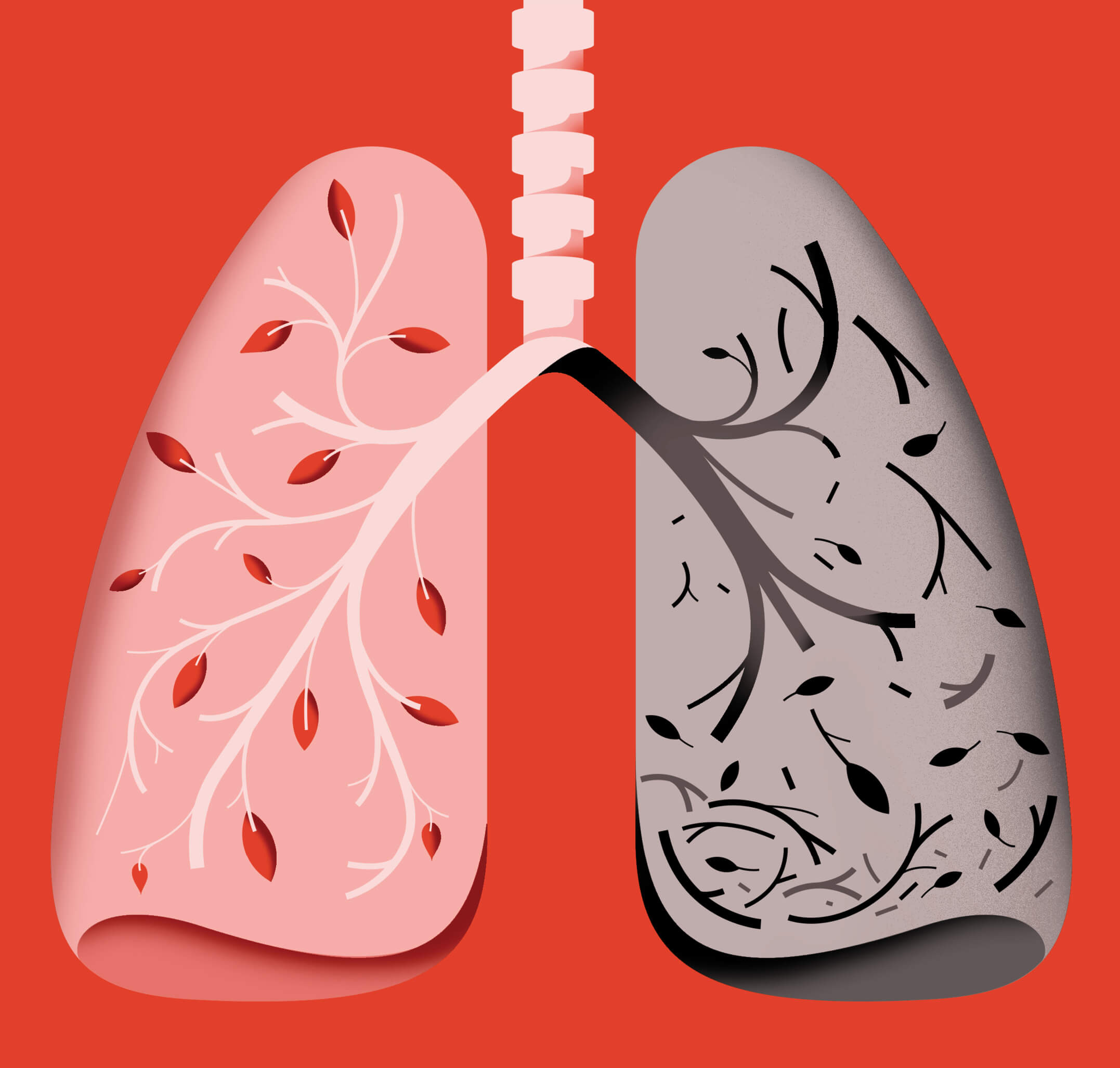
Any respiratory infection, from colds and flu to COVID and respiratory syncytial virus (RSV), can make you feel miserable. But they can also lead to secondary issues, including bronchitis and pneumonia. These two infections may share similar symptoms, but in general they can require different treatments—and pose different risks.
BRONCHITIS: MISERABLE BUT MANAGEABLE
It may start with a cold or flu-like infection that leaves you feeling run-down and achy, says Neil Kalsi, M.D., an assistant professor in the University of Nebraska Medical Center Department of Family Medicine. And with untreated bacterial bronchitis, the infection may worsen, particularly in patients with underlying lung diseases, and the airways leading to the lungs may get further inflamed and filled with mucus. The result can be a nagging cough, which may be wet or dry, that can persist for weeks. Other symptoms can include sore throat and soreness in the chest from coughing.
Since bronchitis is frequently caused by a virus, doctors defer prescribing antibiotics unless a bacterial infection sets in. Instead, helpful tips for feeling better include a cozy blanket, plenty of rest and fluids—especially hot beverages—and that popular home remedy, honey, which may provide temporary relief.
Recovery can take time. “It may not be a day-by-day improvement, but rather a week-by-week improvement,” Kalsi says.
PNEUMONIA: DEEP AND DANGEROUS
While bronchitis affects the larger airways, pneumonia develops in the air sacs of the lungs. It creates inflammation and fluid buildup. And it can be far more dangerous: Pneumonia causes more than 1 million hospitalizations and more than 50,000 deaths each year in the U.S., according to the American Lung Association.
Influenza, RSV, COVID-19 and the common cold virus can all lead to pneumonia. But so too can a common type of bacteria, pneumococcus, which can be spread by coughing, sneezing or touching infected surfaces. Pneumonia can trigger a bad cough as well as other, more serious symptoms, and can include:
▶︎ Fever, shaking and chills
▶︎ Shortness of breath
▶︎ Chest pain
▶︎ Loss of appetite
▶︎ Rapid, shallow breathing
▶︎ Fatigue
▶︎ Confusion, especially in older adults
Chest X-rays, ultrasound, CT scans and other techniques may be used to diagnose pneumonia. A second test is sometimes used to confirm the diagnosis.
Treatment depends on what’s causing the infection—a diagnosis your doctor may make using blood, sputum or urine tests. If it’s bacterial pneumonia, your doctor may prescribe an antibiotic. And in rare cases when pneumonia is caused by a fungal infection, antifungals can help alleviate the illness.
Viral pneumonia, on the other hand, isn’t treated with antibiotics. Some prescription medications can help with the symptoms of viral pneumonia.
WHEN TO SEE A DOCTOR
A fever that’s higher than 101 degrees is a sign you need to see a doctor, says Anthony Szema, M.D., who specializes in pulmonary diseases and clinical immunology at Hofstra/Northwell on Long Island, New York. The same goes if you have chest tightness or feel short of breath, very fatigued or dehydrated.
Let your doctor know what OTC medications you’re taking and ask what changes in your symptoms require a follow-up. Unless you’re diagnosed with bacterial pneumonia, it’s best not to push for an antibiotic. Overuse of antibiotics can have a number of ill effects, including putting you at risk for C. diff, a dangerous infection that can set in when your gut microbiome is compromised—a potential pitfall of antibiotics, especially for older adults.
Bottom line: A seemingly simple infection can take a turn for the worse quickly. Don’t be shy about seeking medical attention.
WINTERIZE YOUR LUNGS
You can do a few things to help reduce your risk of coming down with bronchitis or pneumonia.

VACCINATE
The CDC recommends pneumococcal vaccination for adults 50-plus to help reduce your risk. COVID-19, RSV and flu shots can also help protect you.

WASH UP, MASK UP
Don’t forget about frequent handwashing and face masks, which can help block the spread of germs, including those that can cause bronchitis and pneumonia.

CARE FOR YOUR LUNGS
If you use an inhaler, make sure your prescription is up to date. When necessary, use a spacer device, Szema says. If you smoke, make quitting a priority.

PURIFY
Air purifiers with HEPA (high-efficiency particulate air) filters in your bedroom and common rooms may be helpful in reducing your exposure to viruses.
NATHALIE LEES