Staying Fit


Headed to the doctor’s office or pharmacy this fall to get your annual flu shot, COVID booster or RSV vaccine? Don’t forget about another vaccine that’s critical for older adults to receive — one that protects against pneumococcal disease.
Funny-sounding name aside, pneumococcal disease is serious business. According to the Centers for Disease Control and Prevention (CDC), approximately 10 percent of all patients with invasive pneumococcal disease die of their illness. In fact, pneumococcal disease is one of the most common causes of vaccine-preventable deaths in the U.S., and older adults are among those at higher risk for some of these more severe outcomes.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
What is pneumococcal disease? It’s an umbrella term for any infection caused by the Streptococcus pneumoniae bacteria — pneumonia and meningitis are a few examples. This bacteria spreads when respiratory secretions (think saliva or mucus) are sent through the air by coughing or sneezing and then inhaled.
Streptococcus pneumoniae are particularly lethal for the lungs and can potentially lead to pneumococcal pneumonia, the most common type of pneumonia the U.S. An estimated 150,000 Americans are hospitalized with this illness each year, and it kills about 1 in 20 of those infected.
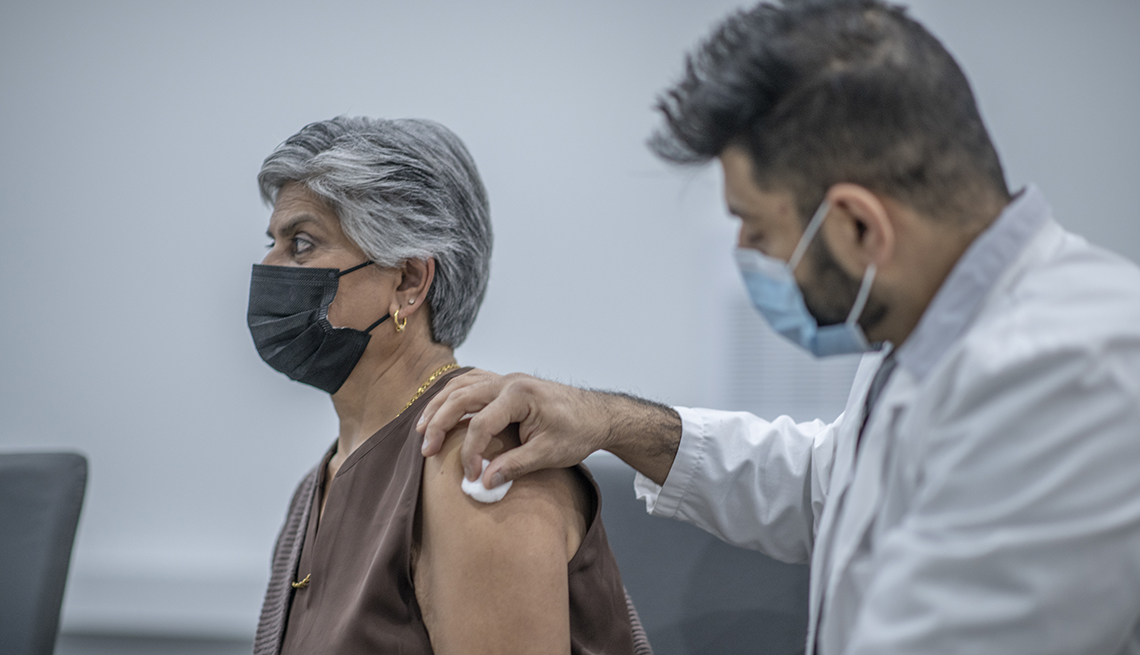
Even with appropriate antibiotics, pneumococcal pneumonia, “particularly in people 65 and older,” has a high case-fatality rate, notes Gregory Poland, M.D., director of the Mayo Clinic’s Vaccine Research Group. A big reason: As we age, the immune system becomes less able to fight off infections.
But studies show the pneumococcal vaccine — which is recommended for adults 65 and older and for individuals with certain medical conditions — can help to lower your chances of contracting the disease or reduce its severity if you do get it, possibly saving you from a stint in the hospital or even death.
That, alone, is a good reason to get the vaccine once you’re eligible. Here are five others.
1. It’s flu season
Flu season is upon us, and experts are expecting this year to be a rough one. That matters because “pneumococcal pneumonia can follow other viral infections, particularly influenza,” notes William Schaffner, M.D., an infectious disease specialist at the Vanderbilt University School of Medicine.
Here’s how: The flu virus attaches to, and infects, the cells lining the mucous membranes in the back of the throat and nose. Normally, the cells eject infectious agents out of the body via the nose or mouth, or they’re simply swallowed. But when impaired by the flu, the cells lining these membranes allow bacteria to slip down into the bronchial tubes and trigger a secondary infection in the lungs.
The infection inflames the air sacs in the lungs and causes them to fill with pus and fluid, making it harder to breathe and triggering a whole host of other unpleasant symptoms.
The flu shot can reduce your likelihood of experiencing this dangerous dual flu-pneumonia infection. So can the pneumococcal vaccine, which unlike the flu shot, isn’t given on an annual basis. For most, one jab will do it, although some adults (those who receive what’s known as PCV15, or the 15-valent pneumococcal conjugate vaccine) require two. That said, if you’re going in for your flu shot and are eligible for your pneumococcal vaccine, the CDC says you can get them at the same time.














































































More on Health
What to Know About the 'Eris' COVID Variant
The omicron spinoff is now the dominant strain
How Long Does a COVID Booster Shot Last?
Get a vaccine when it’s recommended, health experts say
What to Know About the Coronavirus Vaccines
Questions continue as millions of Americans get immunized