Staying Fit
Usually you feel better after you pass a kidney stone. But not long after Timothy Gibbons passed one in December 2022, he woke up one morning with shivers, nausea and terrible pain when he tried to urinate.
Gibbons, 53, a funeral director in Fairview Heights, Ill., thought he probably had a urinary tract infection. But when his heart started racing and his vision blurred, he realized his condition was serious.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
He rushed to the emergency room, where doctors diagnosed him with sepsis.
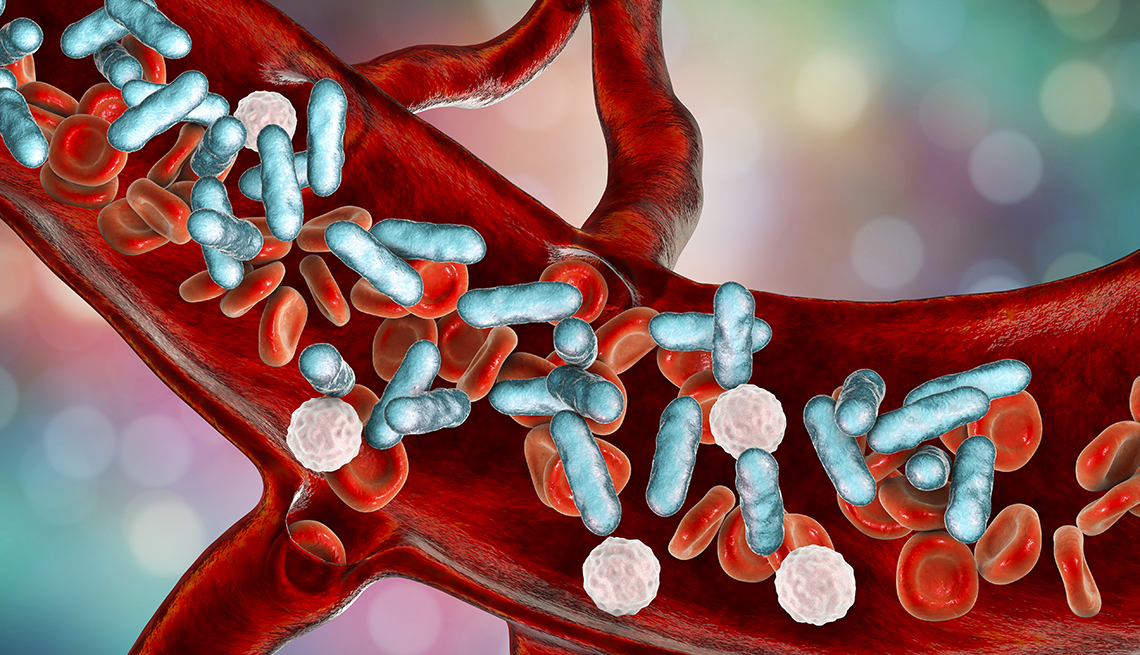
Sepsis is a life-threatening condition that happens when your body overreacts to an infection. It can be triggered by a urinary tract infection, a lung infection or even an infected cut or scrape.
Vaccines lower sepsis risk
Experts say one of the best ways to protect against sepsis is to get all recommended vaccines, including your annual flu, COVID-19 and pneumococcal shots. They can help protect you from infections that lead to sepsis.
More than 1.7 million American adults every year develop sepsis, and as many as 30 percent of them die from the illness.
Older adults are particularly susceptible.
“When they said, ‘You have sepsis,’ I thought I was about to die,” Gibbons says. “As a funeral director, I see that on death certificates all the time.”
A “sneaky” illness
In sepsis, the body’s response to an infection is out of control, creating inflammation and setting off a cascade of problems. Blood pressure drops and blood vessels get leaky, impeding blood flow to important organs such as the heart and brain. “Most of the time when we develop an infection, we can keep it localized where it started. But there are times when the body can’t do that. That’s really what sepsis is,” says Grant O’Keefe, a physician at the University of Washington School of Medicine who has studied sepsis in trauma patients.
Sepsis can be triggered by any type of bacterial or viral infection.
The infection often starts in the lungs, urinary tract, skin or gastrointestinal tract, according to the Centers for Disease Control and Prevention (CDC).
“Particularly in older people, urinary tract infections are a common cause,” says Wesley Self, an emergency medicine physician and senior vice president for clinical research at Vanderbilt University Medical Center. “Lung infections [pneumonia] are also very common.”
Sepsis is treated with antibiotics, fluids and support to vital organs, and early treatment offers the best chance of cure. But sepsis can be hard to detect before someone is seriously ill.
Patients “may not always have clear symptoms,” says Mark Winther, an emergency medicine physician at Bassett Healthcare in Cooperstown, New York. “The reason it’s so dangerous is that it’s sneaky.”