Staying Fit
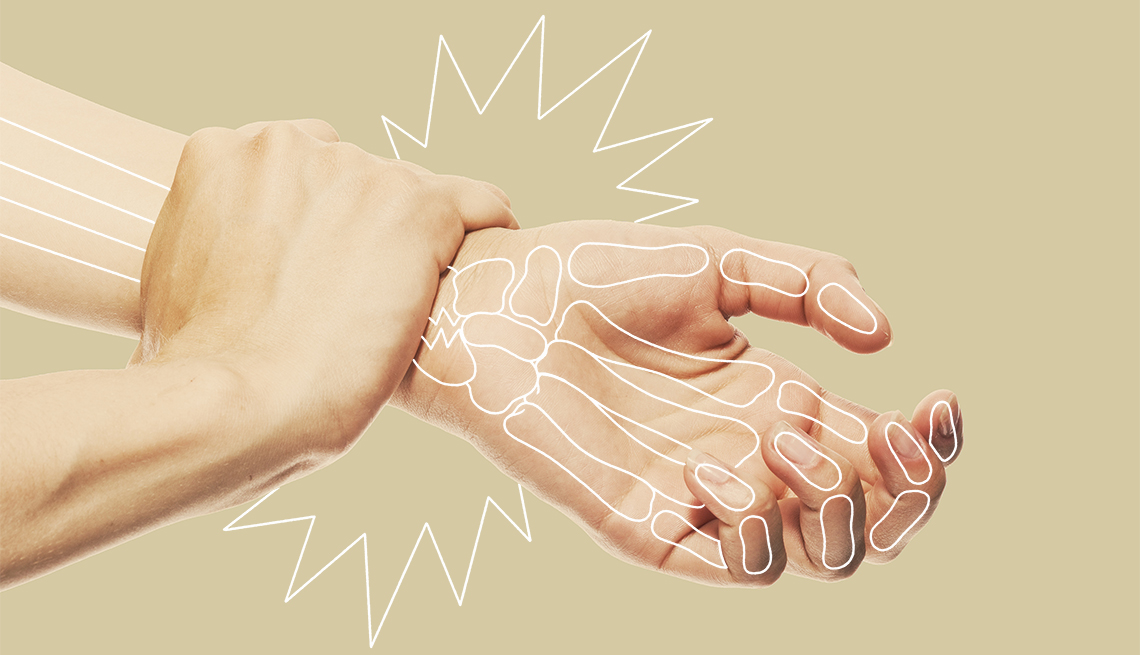
I got my wake-up call about bone health 15 years ago. I was enjoying a stroll around my neighborhood with my dog, Gunther, when I tripped over a crack in the sidewalk. As I fell, I thrust my right hand forward, and when I hit the ground, the pain and swelling in my wrist were immediate. After five decades, I had broken my first bone.
That incident gave me a crash course in bone health. First, I was sent for a bone density test, which revealed that my bones had thinned to the point of osteopenia (think of that as a precursor to osteoporosis, not unlike prediabetes is to diabetes). Then a blood test showed that my vitamin D levels were extremely low, which doctors told me was making it hard for my bones to access the calcium they so desperately needed. Suddenly, without a prior clue, I discovered I was on the express train to osteoporosis.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.


Osteoporosis is often called a silent disease because people who have it may not know until a bone breaks. But it’s not entirely silent, says Andrea Singer, M.D., director of bone densitometry at MedStar Georgetown University Hospital and chief medical officer of the Bone Health & Osteoporosis Foundation (BHOF). These are some of the most common — and surprising — signs that might mean you need a bone check:
- You’re getting shorter. Losing height is one of the most common signs that your spine might be shrinking. Measure yourself annually so you can spot this early.
- Unexplained back and neck pain. Back pain could have many causes, including a compression fracture or collapsed vertebra in your spine.
- Poor posture. If you feel uncomfortable when standing straight or notice a hunch in your upper back, it could be a sign of spinal bone loss or fracture.
- Shortness of breath. If your spine is starting to compress because of bone loss or fracture, your lung capacity may be reduced. Shortness of breath can be a symptom of several other serious issues too; always get it checked.
- Brittle fingernails. Nails that break easily might indicate you don’t have enough collagen in your diet. If your nails have vertical ridges, this could mean you’re not getting enough calcium from what you eat or drink, or your body may not be properly absorbing calcium.
- GI issues. Bone loss is connected to several gastrointestinal conditions, such as celiac disease and inflammatory bowel disease, both of which can inhibit nutrition absorption. In addition, some GI issues require treatment with steroids, which also lower bone density.
- Dental Issues. Tooth loss can be a sign of bone loss in the jaw area, and may additionally indicate bone loss and decreased bone density in other areas of the body. Pay close attention to this sign if you’re losing teeth too easily.
- Weaker grip strength. Having low grip strength is associated with a decrease in muscle strength, an increase in frailty and a heightened risk of falling and fracturing bones. Grip strength can be easily measured in a doctor’s office or at home with a simple tool called a hand dynamometer.
- Weight loss. Being a serial dieter, or losing significant weight or having rapid weight loss, increases your risk for bone loss.
- Broken bones. The most obvious signal of all: Fracturing a bone is a pretty clear sign that your bones are getting weaker.
Know the risks
Paying attention to these early warning signs of bone decline is important; so is knowing your risk of developing the bone-weakening disease. Certain factors can increase the likelihood of developing osteopenia and osteoporosis. Some of them are within your control. Others are not, but you need to be aware of them, too.
1. Age. As you age, your body tends to lose some bone density. But osteoporosis is not inevitable, and it can be slowed or halted with lifestyle changes — exercise and a bone-healthy diet, for example — and medications.
2. Gender. Women are four times as likely to develop osteoporosis as men are, and about half of women and one quarter of men over age 50 will break a bone because of osteopenia or osteoporosis.