Staying Fit
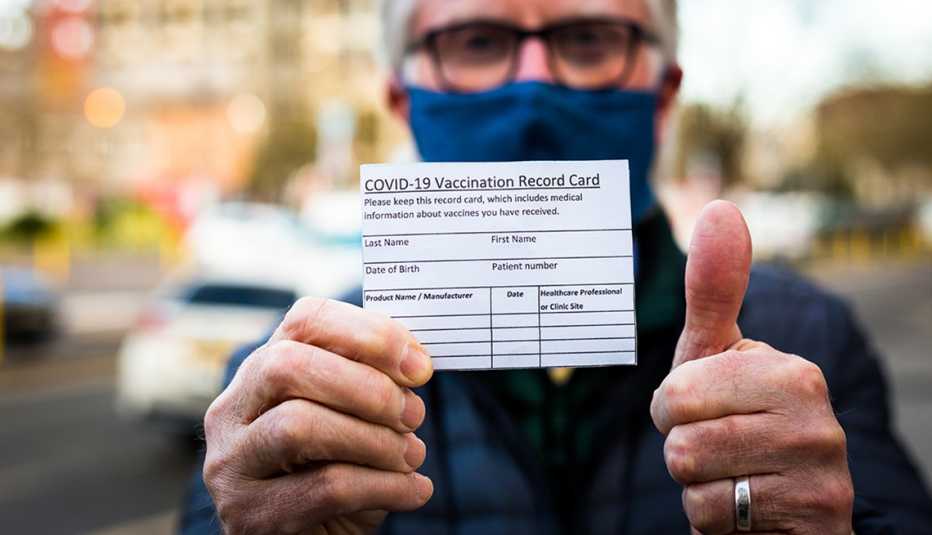
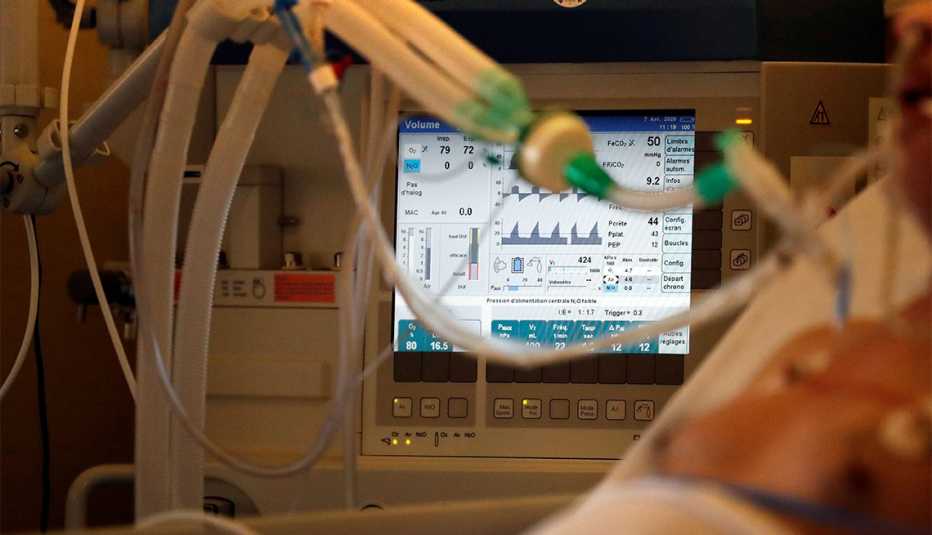
The U.S. may soon have access to two new antiviral pills that are designed to prevent hospitalization and death from COVID-19 in people who are most at risk for developing a serious case of the disease. If authorized, the first-of-their-kind treatments, from drugmakers Merck and Pfizer, could help to curtail the roughly 1,000 daily U.S. deaths still being caused by a coronavirus infection, though experts stress that the vaccines remain the most important tool in the fight against COVID.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
Unlike current COVID-19 treatments that are administered in health care facilities by injection or an IV, these oral antivirals can be dispensed at pharmacies and taken at home, making them more accessible and convenient for patients and health care providers. Data under review by the U.S. Food and Drug Administration (FDA) shows that molnupiravir, the pill from Merck and its partner Ridgeback Biotherapeutics, reduced the risk of hospitalization and death in high-risk patients by about 30 percent in clinical trials. Pfizer’s pill, whose brand name is Paxlovid, was shown in trials to cut risk by nearly 90 percent, the company said.
“It's another tool to add for those people who are at high risk for having hospitalization and death due to COVID-19, and I think it's a really important tool for them,” says Jason Pogue, a clinical professor of pharmacy at the University of Michigan College of Pharmacy and an infectious diseases clinical pharmacist at Michigan Medicine. “But there are some caveats that are going to come with that.”