Staying Fit
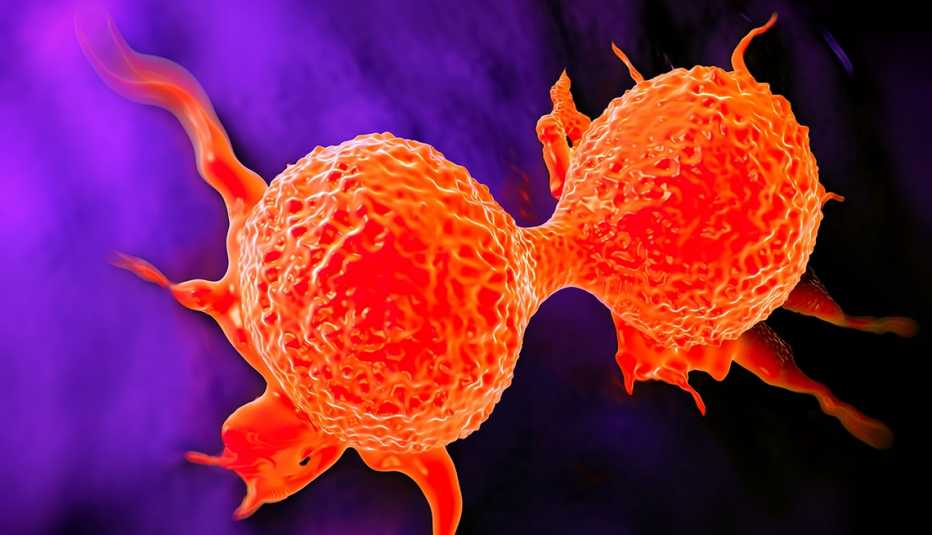
More women, including breast and ovarian cancer survivors and those with specific ancestry, may benefit from genetic testing to determine their cancer risk, says an expert panel that develops health screening guidelines for doctors.
The panel, the U.S. Preventive Services Task Force (USPSTF), has long advised primary care doctors about when to refer women to a genetic counselor to discuss the possibility of testing for mutations in the genes BRCA1 and BRCA2, which are linked to a significantly increased risk of breast and ovarian cancer by age 70.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
In an update published in the Journal of the American Medical Association, the task force expanded on its existing recommendation — that physicians should evaluate a woman's risk if she has a family history of BRCA-related cancer — to include two more groups:
- Women with a personal history of BRCA-related cancer, meaning those who are now considered cancer-free but were previously treated for breast, ovarian, fallopian tube or peritoneal cancer.
- Women whose ancestry puts them at increased risk. This applies primarily to people with Ashkenazi Jewish ancestry, 1 in 40 of whom have a BRCA mutation, compared with about 1 in 500 people in the general U.S. population, according to the Centers for Disease Control and Prevention (CDC).

Know the Numbers
• About 50 percent of women with BRCA1 or BRCA2 will get breast cancer by age 70
• 7 percent of women in the general U.S. population will get breast cancer by 70
• About 30 percent of women with BRCA1 or BRCA2 will get ovarian cancer by age 70
• Fewer than 1 percent of women in the general U.S. population will get ovarian cancer by 70
— Source: CDC
Experts say the inclusion of cancer survivors has particular significance for older adults who were successfully treated for BRCA-related cancer before genetic testing became available in the mid-1990s.
"One of the things that I see very commonly is that people who had cancer a long time ago feel like this information is not particularly helpful,” says oncologist Susan Domchek, executive director of the Basser Center for BRCA at Penn Medicine, “but it still matters."
Testing can help cancer survivors because BRCA mutations put people at risk of others cancers, including those that tend to develop later in life. A woman now in her 70s who was successfully treated for breast cancer in her 40s, Domchek says, may still face an elevated risk of ovarian cancer.


































































