Staying Fit
Andy Markowitz
When the Minnesota Department of Health announced last month that nursing homes and assisted living facilities in the state could allow some family caregivers to resume regularly visiting loved ones, Kathy Merkel broke down: “I heard the press conference, I got up, I cried."
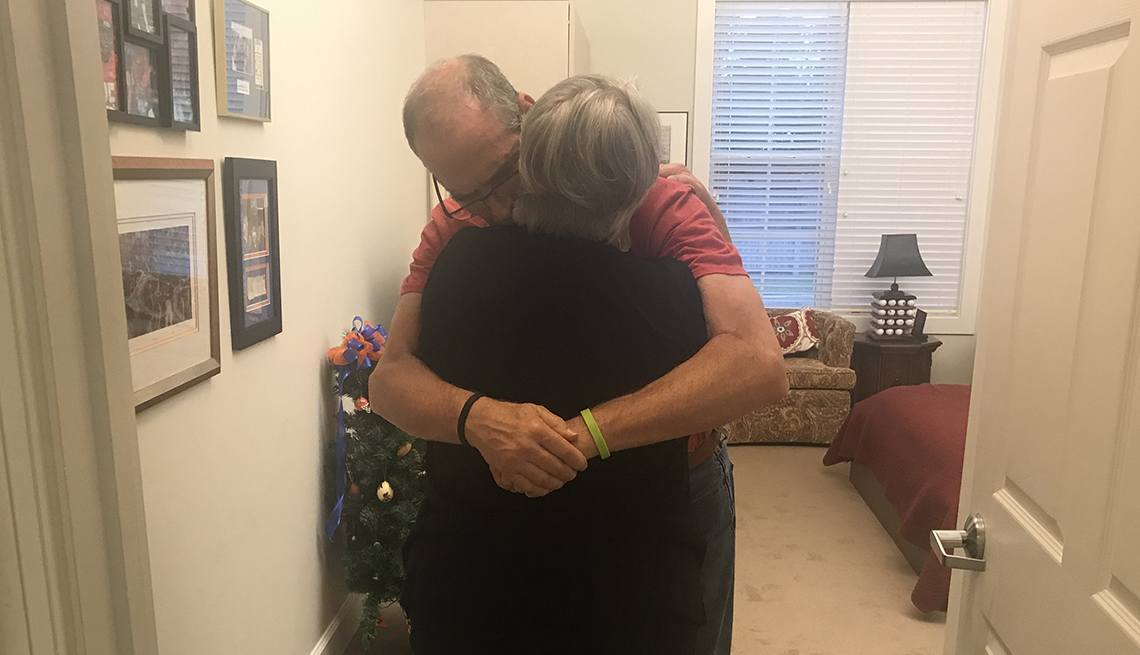
Two weeks later, Merkel entered her mother's northern Minnesota nursing home for the first time in more than four months. She and her brother now come daily, making sure June Merkel, who is 86 and has moderate dementia, eats her meals, gets her hair done and is soothed when she gets anxious and cranky around sundown, as they had done for years before COVID-19 hit.


AARP Membership— $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
"It's a lot of comfort care. She needed us,” Kathy Merkel says. “We're beyond grateful.”
Minnesota is one of a handful of states that have written “essential caregiver” policies into their strategies for resuming nursing home visits after a months-long ban on most visitors because of the pandemic.
In those states, long-term care facilities have discretion to allow regular access to visitors like Merkel, whom they deem critical to a resident's daily care and emotional well-being. These visits are different than most nursing home visits happening these days, which are closely monitored, strictly time-limited and happen in designated common areas, often outdoors, with protocols for masking, distancing, hygiene and health screening.


As pandemic lockdowns at many facilities stretch into their sixth month, the concept of expanded visits for essential caregivers is drawing support from advocates for nursing home residents and from many caregivers — and gaining traction among policy makers.
Last week, New Jersey and South Dakota announced essential caregiver policies, joining Indiana and Minnesota, which launched their programs in June and July, respectively. Michigan's nursing home restrictions do not use the term "essential caregiver" but do allow visits that support residents' daily living activities.
The state programs vary in detail but share a goal of mitigating what Minnesota's plan calls “the unintended consequences of prolonged physical separation and isolation on a resident's overall health and well-being."
"There are some residents that are really experiencing severe distress and decline,” says Lori Smetanka, executive director of the National Consumer Voice for Long-Term Care, a nonprofit advocacy group. “We think that for those residents, there needs to be really targeted access."
The push on visitation comes as long-term care facilities continue to struggle with shortages of staff, testing and personal protective equipment (PPE), and as COVID-19 case counts remain high in much of the country. Long-term care facilities account for more than 67,000 COVID deaths in the U.S. — nearly 40 percent of the nation's death toll.
The American Health Care Association and National Center for Assisted Living (AHCA/NCAL), trade groups for long-term care providers, say federal data show that nursing home cases rose sharply in July after falling through most of June, with increases concentrated in the Sun Belt.
The federal Centers for Medicare & Medicaid Services (CMS), which works with states to regulate nursing homes, continues to recommend strict limits on visitation.
"We would love nothing more than to see residents and families together again,” says Katie Smith Sloan, president and CEO of LeadingAge, an association of nonprofit providers of long-term care and other aging services.
"But without a coordinated federal response to address PPE shortages and a federally funded national testing plan, nursing homes must proceed with caution, carefully consider all the tradeoffs with each visitation strategy, then choose among extremely difficult options."